Health
MakSPH Champions Leadership Boost for Wakiso Health Managers
Published
2 months agoon
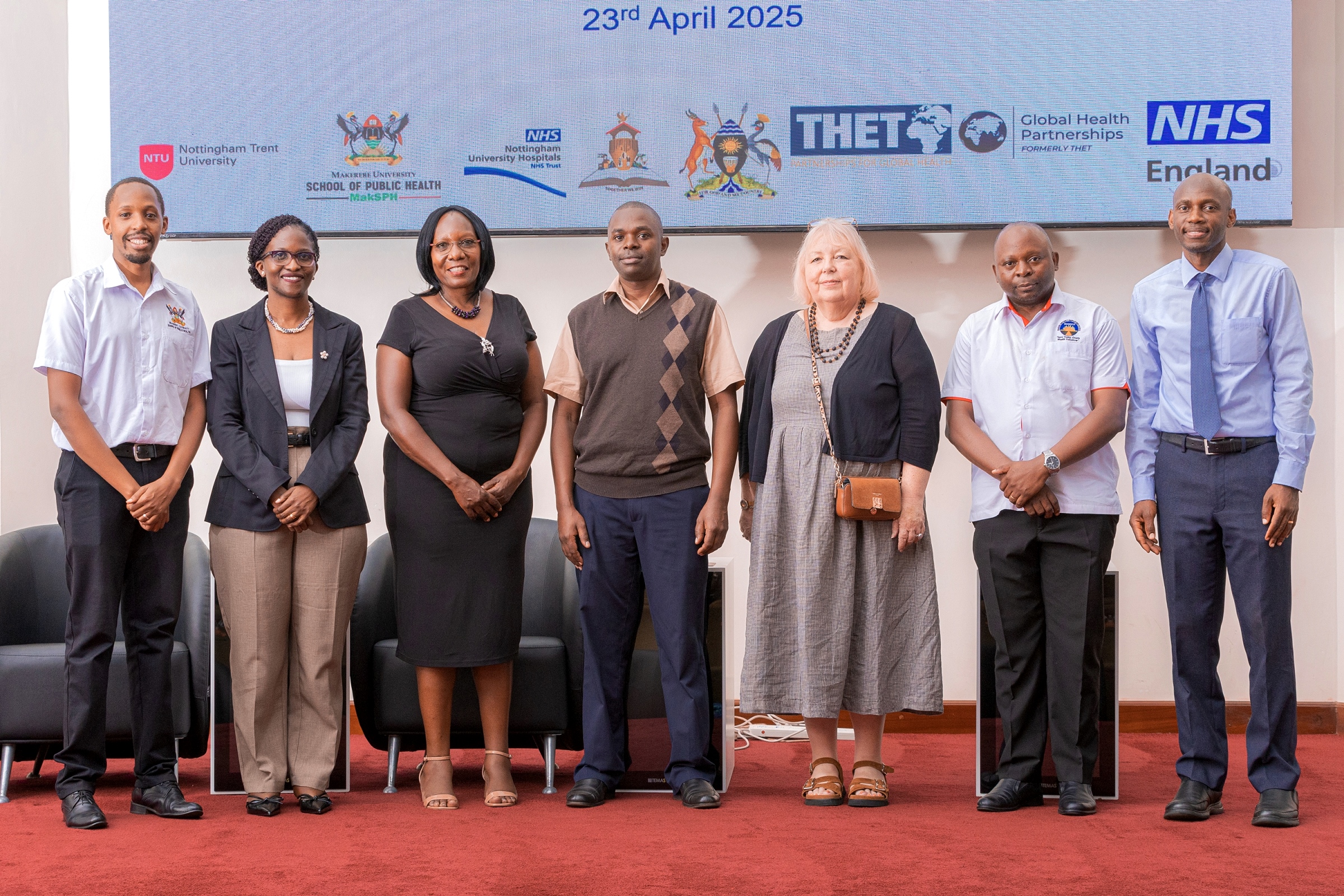
On April 23, 2025, Makerere University School of Public Health (MakSPH) convened district leaders, health managers, and project partners to disseminate the outcomes of a major leadership and management strengthening initiative in Wakiso District, Central Uganda. The one-year project, part of the Global Health Partnerships programme funded by NHS England, was implemented in collaboration with Nottingham Trent University, Nottingham University Hospitals NHS Trust, Wakiso District Local Government, and Uganda’s Ministry of Health.
Launched in 2024, the project titled Strengthening Leadership and Management Among Local Government Health Managers in Wakiso District, aimed to co-design and pilot a leadership and management training tailored to the realities of Uganda’s decentralised health system. The intervention, led by Makerere University’s Dr. David Musoke and Nottingham Trent University’s Prof. Linda Gibson, through the over 15-year-old NTU-Mak Partnership impacting lives in Wakiso, began with a field visit to over 60 public health facilities in the district, a needs assessment within these facilities to identify key priority gaps, and a baseline survey with the health in-charges to establish the initial status of key indicators.
“We have been very fortunate to work with a supportive local government in Wakiso, from the top leadership down. While many projects struggle to engage district teams, our longstanding relationship with Wakiso made collaboration seamless. Although this was our first initiative specifically focused on leadership and management, we hope it will serve as a stepping stone for even more impactful work in the future,” Dr. David Musoke, a Senior Lecturer at Makerere University and the Uganda Project Lead, said during the dissemination workshop, highlighting the key success factors for the leadership and management project.

Initial results from the needs assessment and baseline on leadership and management competencies conducted among Wakiso District health facility supervisors early last year by the project team and shared during the three-day workshop in June 2024, held in Kampala, which kickstarted the six-month structured fellowship programme for 53 health managers in Wakiso, had found critical capacity gaps. Using a tool evaluating 17 leadership and 33 management competencies, only 40% of the managers met the 80% benchmark for leadership, scoring highest in cognitive skills, while just 33% met the required management standard, performing best in self-management and lowest in quality management.
Then, the health facility managers with postgraduate training, longer service, and strong team dynamics, showed overall better performance. While working relationships with subordinates and the district leadership were largely positive, performance was hampered by systemic challenges such as limited resources, low motivation, and weak teamwork. Overall, the study also pointed to a misalignment of expectations between the District Local Government and the Health Ministry, underscoring the need to strengthen coordination to improve services.
The result of this mismatch was to the effect that, as of this time last year, Wakiso District ranked among the bottom 10 on the national health league table, which is an annual Ministry of Health assessment of district performance across key service delivery and patient satisfaction indicators. This was despite Wakiso being Uganda’s most populous district, with over 3.4 million residents today, as it continued to struggle to deliver essential health services to the public. The 2022/2023 Annual Health Sector Performance Report also flagged persistent challenges, including frequent transfers of facility in-charges, overstretched management structures, and weak internal communication and coordination.

It was this stark reality that informed the leadership and management intervention in Wakiso. Officiating the dissemination of the project outcomes, Dr. Sarah Byakika, Commissioner for Planning, Financing, and Policy at the Ministry of Health and a member of the National Oversight Mechanism for the programme, commended the remarkable progress made in just six months, citing visible improvements across the district as a direct result of the intervention.
“I have been involved with this programme right from its inception, and I’m proud that Uganda became one of its major beneficiaries,” Dr. Byakika said with gratitude, commending the strong collaboration between the Ministry of Health, Makerere University, Nottingham Trent University, Nottingham University Hospitals, Wakiso District and the development partners for supporting the initiative. She emphasised the value of this partnership in strengthening leadership and management competencies among Wakiso District health managers to address critical performance gaps in health service delivery.

“Wakiso is Uganda’s largest and most populous district, yet it has long underperformed on key health indices. Despite its semi-urban nature, it faces enormous health service delivery challenges, partly due to the overwhelming burden on its District Health Officer, who oversees more than 60 public and over 340 private health facilities. Many of these private facilities open and close frequently, complicating service oversight,” Dr. Byakika observed with concern.
Her sentiments were echoed by the District Health Officer, Dr. Emmanuel Mukisa, in a message delivered by Wakiso District Biostatistician, Mr. Frank Kakande. He noted that the project had contributed to a noticeable shift in the district’s health system performance, with visible improvements in leadership, communication, and accountability among facility in-charges beginning to translate into better overall health service delivery outcomes.
“You cannot talk about management without addressing performance: they go hand in hand. As someone who sits at the centre of district health data, I can confidently say that performance has improved. During the most recent national local government performance assessment, where I participated in the evaluation, Wakiso District’s health department ranked 18th out of 146 districts. That health ranking is a major achievement. We have consistently performed poorly in the past, but this time, we made significant progress,” Mr. Kakande told the attentive audience, speaking with an air of relief and satisfaction.

The Wakiso District Biostatistician credited part of this progress within the district, from the poor performance last year, to the leadership training and mentorship delivered through the project, citing visible improvements across key health indicators. He stressed the need to sustain this momentum through continued mentorship, internal capacity strengthening, and consistent application of the skills acquired by health managers, particularly in tackling persistent management challenges such as absenteeism, delegation, and accountability.
“Last week, I held a performance review at Kakiri Health Centre III, and the improvements were clear. These management skills are making a difference. You can see the change across indicators. But what matters now is sustainability. The support provided through supervision and mentorship was essential. But it’s up to us to keep the fire burning. We have learned a lot: communication skills, problem-solving, time management, and decision-making. Managers are now communicating better. Even issues like absenteeism are being addressed through proper reporting and action,” Mr. Kakande said.
Earlier, Dr. Musoke, presenting the overall project overview and success, explained that based on initial findings from the baseline and needs assessment, the team co-designed and delivered a structured six-month capacity-building programme targeting 60 health facility in-charges in Wakiso District. The programme blended in-person and virtual sessions, combining practical training with one-on-one mentorship, and included an exchange component between Uganda and the UK to promote international exposure and peer learning. This allowed the health managers to apply new skills to strengthen health outcomes in Wakiso.
“This project rightly focused on addressing gaps in leadership and management. I advocated for including this component in the programme, because our national health review missions consistently show that poor performance often stems from weak leadership and management,” Dr. Byakika affirmed, adding that: “I am pleased to see that nearly all public facilities in Wakiso participated. While the project had a short implementation window, the evaluation already shows encouraging results. Health managers feel more empowered, motivated, and aware of their roles. That’s a significant step.”
For her part, Dr. Sheba Gitta, Uganda Country Director for Global Health Partnerships, formerly Tropical Health and Education Trust, applauded the leadership and management capacity-building initiative in Wakiso as a timely, locally driven intervention. She underscored the value of two-way learning between Uganda and the UK health systems through the programme, noting that Global Health Partnerships works closely with the Ministry of Health to ensure all funded initiatives align with Uganda’s national development priorities.

“What excites me most is that this was not a pre-packaged programme imported from the UK. The training was co-created by partners, based on local realities and needs. That approach reflects strong collaboration between Makerere University School of Public Health and Nottingham Trent University. I thank Prof. Linda Gibson for her continued commitment and Dr. David Musoke for his proactive leadership in bringing this programme to life. Your consistency and quality of work continue to stand out,” Dr. Gitta shared.
While commending the progress made, she cautioned against “pilotism”, as a tendency for promising projects to end prematurely, calling for the model to be scaled up nationally. To support sustainability, she stressed the importance of documenting the training process, outcomes, and costs to inform ministry-level decision-making and long-term adoption.
Dr. Gitta joined Prof. Linda Gibson, the UK Lead for the Project, to encourage the trained managers to become champions of leadership within their facilities and districts, ensuring that the impact of the programme endures beyond its current cycle. She also thanked NHS England and the UK Government for their trust and investment in Uganda’s health system.
You may like
-


Mak Moves to Revitalize Food Technology & Business Incubation Centre to Drive Innovation & Entrepreneurship
-

Ugandan Study Flags Girls and Senior Students as a Mental Health High-Risk Group
-


Makerere’s PIM Centre Concludes Training on Certificate of Financial Implications (CFI)
-


Call for Applications: Responsible Conduct of Research (RCR) Training Course
-


Call For Applications: PhD Fellowship Training Position
-


Makerere Hailed for Its Leadership in Health Policy and Knowledge Systems
Health
Ugandan Study Flags Girls and Senior Students as a Mental Health High-Risk Group
Published
3 days agoon
July 12, 2025
Based on research led by Max Bobholz and colleagues from Makerere University in Uganda, Essentia Institute of Rural Health, and the Medical College of Wisconsin in the United States.
Adolescence is meant to be a time of holistic growth and self-discovery, but for many Ugandan teenagers, this period is becoming a season of silent mental health struggles. A new study published in PLOS Global Public Health has uncovered a silent but growing crisis: nearly one in five Ugandan secondary school students in the study areas have signs of an emotional disorder. These conditions included anxiety, depression, post-traumatic stress disorder (PTSD), and adjustment disorders often involving excessive worry, sadness, fear, or mood instability. Also, one in 20 adolescents exhibited behavioral issues ranging from attention-deficit/hyperactivity disorder (ADHD) and oppositional defiant disorder to substance use and other risky behaviors like alcohol use.
The study, led by Max Bobholz, a PhD candidate in Public and Community Health at the Medical College of Wisconsin, surveyed a sample of 1,953 students aged 10 to 18 years enrolled in eight secondary schools in Iganga district in Eastern Uganda and Mukono district in Central Uganda. This was one of the most comprehensive efforts yet to understand the prevalence and drivers of mental health challenges among school-going Ugandan adolescents.
“We are looking at a generation facing a complex blend of stressors, namely, academic, social, and emotional,” says Bobholz. “Our findings show that certain groups are especially vulnerable, and schools need to be equipped to respond.”
This study results, published on June 12, 2025 was funded by the Swedish International Development Cooperation Agency (SIDA), a government agency of the Swedish Ministry for Foreign Affairs, through the Makerere University Postdoctoral Fellowship to one of the investigators, Dr. Catherine Abbo. Other researchers included Julia Dickson-Gomez, Arthur Kiconco, Abdul R. Shour, Simon Kasasa, Laura D. Cassidy, and Ronald Anguzu.
According to the study, girls bear a higher emotional burden. Researchers found that female students had nearly two times higher odds of suffering from emotional disorders such as anxiety or depression than their male peers.
Dr. Catherine Abbo, an Adolescent Psychiatrist and Associate Professor at Makerere University, attributes this to both biological and socio-cultural factors. “Puberty brings hormonal shifts that can heighten emotional sensitivity,” she explains. “But just as importantly, Ugandan girls often face intense pressure to conform to gender roles while also navigating issues like body image, harassment, and future uncertainty.” The researchers are calling for gender-sensitive mental health interventions, particularly in schools, where early support could help mitigate long-term mental health issues.

Higher associations in older teens?
Age also emerged as a key associated factor, with each additional year increasing the odds of behavioral disorders by 20%. “As adolescents grow older, they are more prone to risk-taking, impulsivity, and resistance to authority,” explains Dr. Simon Kasasa, a senior lecturer and biostatistician at Makerere University School of Public Health.

“Combine that with academic pressure and identity-related stress, and it’s no surprise we’re seeing more conduct issues in late adolescence,” Dr. Ronald Anguzu, an Assistant Professor in the Institute for Health and Humanity at the Medical College of Wisconsin, added. This study raises critical questions about whether and how Ugandan secondary schools support older students as they transition toward adulthood.
The unseen influence of family mental health
The study also found that adolescents with a family history of mental illness had twice the odds of exhibiting behavioral problems compared to those without such a history.
“This speaks to the intersection of genetics and environment,” says Bobholz. “Living in a household with people affected by mental illness can mean instability, stigma, and lack of emotional support, all of which weigh heavily on a developing mind.”
The authors recommend that school mental health screening include family mental health history and advocate for greater collaboration between education and health sectors to support at-risk households.

Private schools: High marks, higher stress?
Interestingly, students in private schools had 1.4 times the odds of experiencing emotional disorders compared to those in public schools. Private schools, often seen as academic havens, may inadvertently be cultivating high-pressure environments. “There’s an assumption that better facilities mean better well-being,” says Dr. Abbo. “But intense academic competition, social isolation, and a lack of trained counselors can create emotional pressure cookers.”
Previous research in 47 secondary schools across five districts (Rakai, Kyotera, Masaka, Lwengo, and Kalungu) in southwestern Uganda found that economic and family support helped reduce absenteeism among adolescent girls in secondary schools. However, this support did not significantly improve behavior or reduce grade repetition. The region, which includes districts like Rakai and Masaka, also faces a higher burden of HIV, adding to the challenges young people experience.
Meanwhile, a review of data from 42 primary schools in Luwero District identified school-based mental health interventions such as cognitive behavioral therapy and mindset-building approaches as being particularly effective. Researchers now suggest that integrating these strategies, along with efforts to reduce school violence, could go a long way in improving the mental health of Ugandan adolescents.
A-Level pressure: Academic ambition meets mental health strain
The study also found a correlation between advanced (A’level) education and increased risk of emotional disorders. “We selected one school district from each region based on population and past academic performance. As these students prepare for university or the job market, the pressure to succeed becomes enormous,” says Kasasa. “They’re facing a future full of uncertainty, with very little structured mental health support to help them cope.”

A wake-up call for Uganda’s education and health systems
The authors of this study assert the urgent need for school-based mental health programs, especially in private and A-level institutions. These programs should offer routine screening, emotional support, and training for teachers to recognize warning signs of mental health disorders.
Importantly, this study adds weight to calls for a national adolescent mental health policy, tailored to Uganda’s context, with interventions that bridge health, education, and social services.
“Our data shows that mental health challenges are not a fringe issue,” says Bobholz. “They are widespread, significant, and deeply tied to school, home, and society.”
The COVID-19 school closures between 2020 and 2022 deepened feelings of isolation and financial strain, with out-of-school adolescents reporting depression rates as high as 21.5% to 50% higher than their peers who remained in class, according to research published in February 2025. Yet Uganda invests less than 1% of its health budget in mental health, with just one psychiatrist per million people, leaving many teens to cope through cheap alcohol used by 28% of urban youth or untrained healers, as reported by the government paper The New Vision in April 2025. With only 26% of students completing lower secondary school and 35% of the population under age 24, these mental health challenges now pose a serious threat to the country’s future.
Mercy Akankunda of Proven Foundation, a Ugandan NGO supporting vulnerable groups, warns that mental health struggles are quietly eroding the well-being of the country’s youth, over 12 million strong and making up 35% of the population. “These teens are not just statistics. They are the future of Uganda, she asserts. If Uganda hopes to reap the dividends of its young population, addressing adolescent mental health must become and remain a national priority, not just for treatment, but for prevention, resilience, and hope.
Reference:
Bobholz, M., Dickson-Gomez, J., Abbo, C., Kiconco, A., Shour, A.R., Kasasa, S., Cassidy, L.D., & Anguzu, R. (2025). Correlates of behavioral and emotional disorders among school-going adolescents in Uganda. PLOS Global Public Health. Read the study here
Health
Call for Applications: Responsible Conduct of Research (RCR) Training Course
Published
4 days agoon
July 11, 2025By
Mak Editor
The Responsible Conduct of Research (RCR) Training Course, scheduled to take place from July 30th to August 1st, 2025, at the Makerere University College of Health Sciences’ Conference Room.
Background
The SUSTAIN: Advancing Makerere University Masters of Health Sciences in Bioethics program at Makerere University College of Health Sciences aims at developing and institutionalizing a mentorship program in research ethics that facilitates development of bioethics professionals and health researchers who are committed to the growth and application of research ethics in Uganda’s academic and research institutions to the highest possible degree. The Responsible Conduct of Research (RCR) course is one of the short courses that introduces trainees to a framework that involves application of established scientific, professional norms and ethical principles in the performance of all activities related to scientific research.
Course objectives
At the end of this course, trainees should be able to identify, manage and prevent research misconduct.
Course outline
Introduction to RCR; Introduction to Professionalism and Ethics; Human subject’s protection and regulatory framework in Uganda; Humane handling of animal research subjects; Conflict of interest;
Responsible laboratory practices; Mentor-mentee relationships; Collaborative research international, industry); Peer review; Research misconduct (including policies for handling misconduct); Community involvement during research in a low resource setting; Responsibility to society and environment; Responsible financial management; Data acquisition, management, sharing and ownership; Responsible authorship, publication and communication.
Target group
The Responsible Conduct of Research course is targeted at Researchers, Research administrators, Research assistants, Study coordinators, Graduate students and Student supervisors. Certificates will only be awarded to participants with 80% attendance.
Course fee: 205,000/=, or 56USD is payable.
The course fee will cater for meals and refreshments during the training period.
Payment & Registration procedure:
9030026194023, Stanbic Bank, Mulago, Makerere University Biomedical Research Center Limited
Dollar Currency:
9030026194147, Stanbic Bank, Mulago, Makerere University Biomedical Research Center Limited
Please Note: Share payment details on email/whatsup and a hardcopy deposit slip delivered on the first day of the training to Miriam Musazi, Department of anatomy, Bioethics Centre, Room C4,
Mob: +256 782 363 996/ +256 701 363 996, Email: mmusazi@gmail.com.
NB. Only those who will have paid by this date will be considered for the course
Venue: The training will take place at Makerere University College of Health Sciences’ Conference room
Health
Call For Applications: PhD Fellowship Training Position
Published
5 days agoon
July 10, 2025By
Mak Editor
Background:
Makerere University College of Health Sciences (MakCHS), Kampala, Uganda and Global Health Uganda (GHU); in collaboration with other research consortium partner institutions, including, Kenya Medical Research Institute (KEMRI), Kisumu, Kenya; Training and Research Unit of Excellence (TRUE), Blantyre, Malawi; University of Bergen, Bergen, Norway; University of Amsterdam, The Netherlands; and Liverpool School of Tropical Medicine (LSTM), UK have been conducting clinical research on Malaria Chemoprevention. This research has focused on Malaria Chemoprevention in vulnerable patient populations, including children with severe anaemia, children with sickle cell anaemia and pregnant women. As an example, two of our recently completed studies are “The post-discharge malaria chemoprevention in children with severe anaemia [https://pubmed.ncbi.nlm.nih.gov/33264546/] and Malaria chemoprevention in children with sickle cell anaemia [https://pubmed.ncbi.nlm.nih.gov/39718172/]”.
With support from the UK Research and Innovation (UKRI) body, the consortium is expanding these studies to children with severe acute malnutrition, by conducting a large multi-centre randomized controlled trial entitled “Chemoprevention of malaria in the postdischarge management of children with severe acute malnutrition in Malawi and Uganda”.
In Uganda, the study will be conducted at one or two of their study sites in Jinja Regional Referral Hospital, Hoima Regional Referral Hospital or Kitgum General Hospital. Makerere University College of Health Sciences (MakCHS) and Uganda and Global Health Uganda (GHU) seek to appoint a full-time PhD Fellow, on this study. This will be a 4-year post, tenured at Makerere University and hosted at MakCHS.
Expectations of the PhD fellowship:
The PhD fellow will:
- Be a part of the main trial team, and participate fully in its implementation. However, he/she will be expected to design and develop his/her PhD research project, nested in the main trial.
- The area of study will be around “interactions between anaemia and severe acute malnutrition (SAM) in children or the interactions between malaria and severe acute malnutrition in children”.
- Conduct rigorous research, leading to high quality scientific publications.
- Submit a full research concept and obtain registration in the University by end of year-one. As such, there be an initial appointment for one year, renewable upon satisfactory performance.
- Academic mentorship and supervision will be provided by the research consortium (see above – composed of national and international researchers).
- Doctoral scholarly support and training environment, as well as didactic training in research methods and scientific writing skills will be provided by Makerere University.
- The funding support will cover tuition and a competitive monthly stipend for 4 years, scientific conferences fees/travel and other research-related costs.
Prospective candidates must:
- Hold Master’s of Medicine in Paediatrics and Child Health from a recognized university, and licensed to practice medicine in Uganda by the UMDPC.
- Possess undergraduate training in Medicine and Surgery (MBChB/MBBS/MD).
- Willingness to fully commit time and effort to their PhD studies, expected to start immediately
- Candidate should not hold other/concurrent fellowships
- Having publication experience will be an added advantage.
- Be highly motivated and willing to commit to a career in research and academia.
Application procedure:
Interested applicants should submit their application and supportive documents – listed here below, in one PDF document, in an email titled “PDMC-SAM–PhD Fellowship Application” to hr@globalhealthuganda.org [and cc – chdc.desk@mak.ac.ug] by 25th July 2025. The documents should include the following:
- An application letter (Max. 1 page)
- Motivation statement (Max. 500 words)
- CV (Max. 2 pages), including a list of publications
- Two (2) recommendation letters
- Academic transcripts and certificates for all university qualifications
- A synopsis focusing on the proposed PhD research work, describing briefly what is already known/burden, challenges, the gaps and potential interventions (include references) [Max. 800 words].
Trending
-

 Education2 weeks ago
Education2 weeks agoAdmission List to Bachelor of Education External (BED) 2025/26 -Private Sponsorship
-

 General1 week ago
General1 week agoRe-advert: Admission to Undergraduate Programmes 2025/2026
-

 General2 weeks ago
General2 weeks agoAdmission Lists -Disability and District Quota Schemes 2025/26
-

 General2 weeks ago
General2 weeks agoDiploma/Degree Holders Scheme – Self Sponsorship Admission Lists 2025/26
-

 General6 days ago
General6 days agoRe-Advert for Applications for Diploma and Certificate Training
