Health
We Are Pushing Nature to the Edge—But Solutions Are Within Reach: Global Conversations on Sustainable Health
Published
12 months agoon
By
Mak Editor
By Davidson Ndyabahika and Johanna Blomgren
We’ve all done it—tossed leftovers, ignored wilted greens, or shrugged at a half-eaten meal. Food waste is a quiet guilt we all share, a reflex in a world of abundance and scarcity. But what if this small act connects to a larger global issue? On February 26, 2025, experts from Uganda, Sweden, and beyond gathered in a virtual seminar, asking, “How can we nourish ourselves without harming the planet?” Hosted by the Centre of Excellence for Sustainable Health (CESH), the discussion revealed a harsh truth—our food habits are draining the Earth.
The discussion on sustainable food systems marked the beginning of the annual four-part global conversation on sustainable health, organized through a collaboration between Sweden’s Karolinska Institutet and Uganda’s Makerere University under the auspices of CESH.
In Kampala, the paradox is stark. Every day, 750 tons of food waste fill the city’s landfills, enough to feed thousands. Rotten mangoes spill from crates in Nakasero Market, and half-eaten Rolex wraps pile behind street stalls. Uganda’s Food Rights Alliance shows 37.8% of this waste comes from plates and markets. Across East Africa, organic waste, like spoiled vegetables and discarded tubers, makes up 79% of urban trash—a grim reflection of broken systems. Beyond this is a city stuck with piles and piles of organic trash, which has previously been fatal with a slide in one of Kampala’s major landfills. Meanwhile, 26% of Uganda’s children remain stunted.
At the heart of this week’s global conversation was the WWF’s Living Planet Report 2024, a sobering revelation of a 73% decline in global wildlife populations since 1970. Freshwater ecosystems have hemorrhaged 85% of biodiversity, Latin America’s species richness has plummeted by 95%, and Africa—home to smallholder farmers who feed millions—has lost 76%. “Nature is disappearing at an alarming rate,” warned Harold Turinawe, WWF Uganda’s Forest Markets Transformation Manager, his voice weighted with urgency.
“We are pushing Earth’s systems to irreversible tipping points, and despite the increase in food production and land use and the destruction of habitats, the world is still hungry; we have over 735 million people going to bed hungry every other night. The contradiction is striking,” Turinawe added.

The report highlights the Amazon’s lush canopies that are felled for cattle ranches. The interplay of man’s unsustainable utilization of Mother Nature, leading to the food paradox, feast, famine, and ecological ruin, underscores the urgency of addressing global goals in a coordinated manner.
The report’s indictment of industrial food systems is clear: agriculture claims 40% of habitable land, 70% of freshwater, and drives 25% of greenhouse emissions. Yet, 735 million people still starve nightly. “Our obsession with monocultures and processed foods isn’t just destroying habitats—it’s failing humanity,” said Dr. Rawlance Ndejjo, the seminar’s moderator and a public health lecturer at Makerere University.
Florence Tushemerirwe, a Ugandan public health nutrition expert based at Makerere University’s School of Public Health, pointed out the irony: 26% of children are stunted, while obesity rises among adults in Uganda. “We grow nutrient-rich crops but export them, leaving people dependent on cheap, processed imports. In fact, many people do not appreciate their nutrient value,” she said. Uganda’s iodine-depleted soils now rely on fortified foods—a temporary fix for a growing crisis.

All through the seminar, the message was clear: we are wasting abundance while ecosystems crumble and people go hungry. “Our salt is iodized because our soils no longer provide it. Biodiversity loss isn’t abstract—it’s stealing nutrients from our plates. But if we don’t maintain our nature’s health, or our environmental health, or our natural resources health, it means that whatever food we grow, we actually do not carry the nutrients we need to maintain a diverse diet,” said Tushemerirwe.
The panel dissected global food trade’s role. WWF’s Turinawe lamented, “90% of deforestation is for agriculture. In Uganda, the once-vibrant wetland ecosystems of Lwera at the shores of Lake Victoria now face severe degradation due to large-scale rice growers; in the Amazon, its cattle ranches.”
Dr. Rachel Marie Mazac of Stockholm Resilience Centre stressed Europe’s complicity: “Sweden’s ‘virtual biodiversity loss’—importing deforestation via beef and soy—shows how our diets export destruction.”
“From a Swedish perspective, we are highly dependent on imports, particularly raw materials, which contribute significantly to biodiversity loss in other regions. It’s difficult to pinpoint the exact impact, especially with biodiversity, but there’s a concept of “virtual impact,” says Dr. Mazac.

Food consumed in Sweden, though produced elsewhere, contributes to biodiversity loss in those areas. The issue links to trade, food production, and distribution. It’s not just about production or waste but also equitable distribution.
Dr. Ndejjo added starkly, “You could be eating a burger from a cow grazed on razed Amazon forest. Guilt isn’t enough—we need systemic change.”
Amid the grim statistics, the panelists outlined a roadmap for redemption: nature-positive agriculture, subsidy policy reform, improved localized diets, global accountability, and honest discussions on the GMO dilemma.
Turinawe emphasized the need for agroecology in extension services—integrating trees, crops, and livestock to rebuild soil health and biodiversity. He stressed while critiquing Uganda’s Parish Development Extension Model for prioritizing enterprises for profit over sustainability. “We are saying get one million to a farmer. What are they producing? They are engaging in commodities that are predetermined. Nobody’s talking about Mother Nature. Who takes care of the soil? Who takes care of the water needs? Who takes care of the diversification we are talking about? But diversification in the diet begins with diversification on the farm. So my first issue is strengthening the agricultural extension services,” says Turinawe.
Adding that things like soil health management, land tenure system farmer-to-farmer network for peer learning, and fair farmer subsidies should be key to planning and agricultural extension.
“In Uganda, where I come from, and currently in Kampala, if you head north towards Zirobwe in Luweero District, you’ll find people we call Bibanja owners—essentially squatters who don’t own the land they occupy. These individuals cannot engage in sustainable agriculture as we’re discussing; their focus is survival. What we need are programs that give farmers secure land rights, which can motivate them to invest in soil health and environmental conservation—investments that take time. Improving soil is not a short-term effort; it requires long-term actions like planting trees, integrating practices, and using farmyard manure. None of this is realistic for someone who fears being displaced tomorrow. We need to approach this challenge collectively.”
Subsidies must reward sustainable practices, not industrial giants.
“Why not tax breaks for farmers using organic manure?” Turinawe challenged. “I would love to hear that a farmer that is engaged in sustainable cocoa production and coffee production gets a tax holiday rather than having a blanket of investors getting a holiday. Put subsidies and investment incentives in the right direction. We shall spur production, and of course, this will also bring in corporate partnerships, and we can make our supply chains safer, better, more green, and more sustainable,” Turinawe added.
Dr. Mazac noted that “nature-positive production can feed the world by optimizing crops, livestock, and wild fisheries, and supporting aquaculture that works with wetlands, not against them.” For Mazac, policy is key: She is also an advocate of subsidies and taxes that benefit farmers. Those that ensure incentives that improve soil health and maintain water quality as well as tackle climate change in order to make sustainability profitable.
“We must rethink trade to avoid widening the gap between food-producing areas and markets and instead support local farmers. Subsidies and taxes should empower these communities to nourish their populations before focusing on exports. While exports generate income, they also have significant impacts. A possible solution is changing production systems, but we must also shift dietary and consumption habits, making this a collective effort, not just an individual responsibility.”
Tushemerirwe is hungry for reviving indigenous crops and regulating predatory marketing. “Awareness is power. We must teach communities to value their traditional foods over processed substitutes.”
“There is good food grown in rural areas and available in markets, but people don’t recognize its value due to lack of guidance. We need food-based data guidelines to raise awareness. The Uganda Ministry of Health has a draft for this, along with draft policies to regulate unhealthy food marketing, especially to children. Junk food is advertised everywhere: hospitals, schools, and even street billboards, with fast food chains clustered together. We must regulate this and educate people on the nutritional benefits of eating what they grow over imported alternatives,” she stated.
Dr. Ndejjo believes these draft guidelines to regulate unhealthy food marketing should be finalized into policies and urges policymakers and implementers to prioritize the urgent need for these documents.

The conversation also weighed in on the genetic engineering in agriculture for increased crop yields, popular for GMOs, a dilemma that panelists called for their democratization rather than demonizing them. While Dr. Mazac cautioned against corporate-controlled seeds, Turinawe acknowledged their potential: “If democratized, drought-resistant crops could save farms in a warming world.”
Dr. Mazac noted that while in Europe and the European Union, they are not allowed to grow or sell foods that have been genetically modified, the essence of them should not be overlooked, since they are a technology that seeks to solve the future food crisis.
“GMOs aren’t inherently evil. Drought-resistant crops could save farms—but corporate patents trap farmers,” she said.
Turinawe added, “Our approach to GMO’s is a measure one bordering more on ethics and responsible use of GMOs; we see GMOs as a tool to promote resilience, especially since everything has changed—the food we once relied on can no longer grow in the same way. If GMOs help improve crop resilience, that’s a valuable tool. However, there are concerns that companies like Monsanto could use the GMO technology as a tool of exclusion, e.g., the fear of monopolizing future seed markets. This is where caution is needed.”
A Call for Radical Collaboration
The seminar’s resounding theme was unity: multi-sectoral collaboration is non-negotiable. From street food vendors to policymakers in the boardrooms, every actor must align. “Food systems aren’t siloed,” Dr. Mazac asserted. “They’re woven into climate, economy, and culture.”
“I think we need to sit and agree and engage quite regularly and find solutions for us to be able to produce food but sustainably,” concluded Tushemerirwe.
The Path Ahead
CESH’s global conversations on sustainable health are a microcosm of a global awakening, especially in tracking progress to meet our goals for 2030 and beyond: This seminar on food systems emphasizes the interconnectedness of food security and biodiversity. With the next UN Climate Summit (COP29) on the horizon, the panel’s message is clear—transformative change is possible, but only through courage, equity, and an unyielding reverence for nature.
To find more about this global conversation on sustainable health and more, visit CESH.health
Davidson Ndyabahika and Johanna Blomgren are the co-organisers of the global conversation on sustainable health

You may like
-


Makerere University commemorates 13 transformative years of partnership with Mastercard Foundation
-


Celebrating Academic Excellence: CoBAMS Presents 975 Graduands at Mak 76th Graduation Ceremony
-


Mak 76th Graduation Ceremony: CoNAS Presents 16 PhDs & Best Performing Male Student in the Sciences
-


Medical graduates urged to uphold Ethical values
-


CAES Presents Overall Best Performing Student in the Sciences & a Record 28 PhDs at the 76th Graduation Ceremony
-


Over 9,200 to graduate at Makerere University’s 76th Graduation
Health
MakSPH Environmental Health Graduates Trained to Prevent Disease at Its Source
Published
1 week agoon
February 24, 2026
In most health systems, attention turns to illness after it appears in clinics and hospitals. Environmental Health works earlier, often invisibly, by preventing disease before treatment becomes necessary. At Makerere University School of Public Health (MakSPH), this preventive philosophy shapes the training of students learning to manage health risks at their source, through sanitation systems, safer environments, community engagement, and evidence-based public health action.
This year, as MakSPH presents 29 graduands approved by the Makerere University Senate for the award of the Bachelor of Environmental Health Science (BEHS) degree, four outstanding students graduate with first-class honours. Their journeys, shaped by different personal histories and professional ambitions, provide a clear view of how the School prepares practitioners whose work begins long before patients reach health facilities. Through academic training, field practice, research exposure, and leadership experience, the programme equips graduates to address the environmental and social conditions that determine health outcomes across communities.

Environmental health occupies a distinctive position within public health practice. Rather than focusing primarily on diagnosis or treatment, practitioners work at the intersection of science, policy, and society, addressing risks linked to water and sanitation, food safety, occupational health, climate change, and urbanisation. The discipline demands technical competence alongside communication, systems thinking, and community engagement, capabilities that increasingly define modern public health leadership.
The journeys of Nakulima Bushirah, graduating with a CGPA of 4.58 on February 25, 2026, Mujurani Alphersiiru with 4.44, and Cherop Eric with 4.41, alongside Phillip Acaye, the cohort’s overall best student with a CGPA of 4.63, demonstrate how MakSPH shapes students from varied beginnings into professionals grounded in prevention. Their paths reveal a shared formation that links classroom learning with real-world health challenges and prepares graduates to prevent disease before it occurs.
Bushirah Nakulima’s Turn Toward Prevention

For Bushirah Nakulima, environmental health began during a period of uncertainty. The COVID-19 pandemic repeatedly disrupted her Bachelor of Pharmacy studies at Kampala International University, prompting reflection about the kind of health professional she wanted to become. A conversation with a family friend working in preventive health introduced an alternative path, one focused not on treating illness after onset but on preventing it altogether.
“When I applied to Makerere University in 2022, I was considering two career paths,” she recalled. “I prayed to Allah to guide me toward the best one. When I was admitted to the Bachelor of Environmental Health Science, I accepted it wholeheartedly, and I came to appreciate it even more as I studied.”
Her academic foundation had already demonstrated consistency. She progressed from Melody Junior School in Nansana, where she obtained aggregate eight in 2010, to Shuhada’e Islamic School in Nyamitanga, completing O-Level with 25 aggregates in 2016 and A-Level with 10 points in 2018. Pharmacy initially appeared the logical continuation, yet environmental health offered something broader in scale and impact.
“Environmental Health offered an opportunity to prevent illness and suffering before it occurs,” she explained. “It allows a single intervention, such as WASH or health education, to protect many people at once, and it provides flexibility to work across diverse environments. It offered freedom to operate in various settings, which truly connects with my personality since I love exploration.”
At MakSPH, classroom concepts quickly translated into practice. During her internship at Mukono Municipal Council, she conducted school health education sessions, participated in inspections of markets and abattoirs, and engaged communities facing sanitation challenges. Field exposure deepened her understanding of how environmental conditions directly shape disease patterns, reinforcing prevention as both a scientific and social responsibility.
Leadership further expanded her training. Serving as the 90th Female Guild Representative Councillor (GRC), she represented the School of Public Health in the Student Guild structure, facilitating engagement between students and School leadership on academic and welfare matters. The role strengthened her capacity for representation, negotiation, and collaborative problem-solving, skills central to public health practice, where advocacy and systems engagement are inseparable from technical expertise.
Graduating with a CGPA of 4.58, Bushirah’s research examined roadside vendors’ exposure to air pollution in Kampala, reflecting growing concern about occupational and urban environmental risks. She now plans to pursue advanced training in public health, building on MakSPH’s emphasis on evidence-driven and community-centred practice.
Cherop Eric’s Return to the Classroom

Eric Cherop’s journey into environmental health began not in lecture halls but in community service. Raised in Kapchorwa District, he was shaped by economic hardship and resilience, experiences that informed his commitment to community well-being.
He completed his Primary Leaving Examinations at Chema Primary School, a Universal Primary Education institution, attaining 24 aggregates in 2008. He later joined Sipi Secondary School, where he obtained 37 aggregates at Uganda Certificate of Education in 2012 and continued at the same school for A-Level, earning 8 points at Uganda Advanced Certificate of Education in 2014.
After earning a Diploma in environmental health sciences from Mbale School of Hygiene between 2015 and 2017, he entered public service as an Environmental Health Officer and Community Field Facilitator with Kapchorwa District Local Government. His work included sanitation campaigns, climate resilience initiatives, nutrition education, and household behaviour change programmes. Over time, field experience revealed the limits of practice without deeper theoretical grounding.
“I wanted to understand not only what works in communities, but why it works,” he explains. Enrolling in the BEHS programme at MakSPH in 2022 allowed him to connect practical experience with analytical training. Coursework strengthened competencies in environmental risk assessment, participatory engagement, and data-driven planning. Mentorship reshaped how he interpreted evidence.
“My lecturers helped me move beyond seeing data as numbers,” he said. “I learned to see it as evidence that guides decisions and improves accountability.” Graduating with a CGPA of 4.41, Eric now aims to advance evidence-driven leadership at the intersection of climate change, nutrition, and environmental health, ensuring interventions remain grounded in community realities.
Mujurani Alphersiiru’s Path into Environmental Health

For Mujurani Alphersiiru, Environmental Health arrived at an unexpected moment, when his academic future appeared uncertain. Financial pressures had begun to threaten the continuation of his Bachelor of Nursing Science studies at Kampala International University Western Campus, raising the real possibility that his university education might end prematurely. The turning point came when the government district quota admission list was released, offering him placement at Makerere University under Bunyangabu District and opening an alternative academic pathway he had not previously considered.
At the time, environmental health was unfamiliar to him. “I didn’t know what environmental health was,” he recalls. “But I celebrated because I had reached my dream university.” Orientation sessions and early coursework gradually reframed that uncertainty, revealing a discipline grounded in prevention, systems thinking, and public health policy. What began as an unexpected opportunity soon developed into a clear professional direction.
Serving as class president and 90th Male GRC for the School with Nakulima Bushirah, Mujurani organised student activities, mobilised community outreach initiatives, and advocated for improved learning environments. Balancing leadership responsibilities with academic performance required deliberate discipline and time management.
His educational foundation began at St. Augustine Butiiti Demonstration Primary School in Kyenjojo, where he scored 12 aggregates in 2014. He later attended Pride Secondary School in Mityana, attaining 25 aggregates at O-Level in 2018, before proceeding to Kibiito Secondary School in Bunyangabu, where he obtained 13 points at A-Level in 2021, performance that earned him government sponsorship for university education. At MakSPH, faculty mentorship further strengthened both his academic rigour and commitment to public service.
“Government sponsorship meant responsibility,” Mujurani said. “I had to plan my time carefully while remaining active in school programmes.” Graduating with a CGPA of 4.44, his interests now centre on governance and accountability within health systems, particularly strengthening the implementation of public health policies.
Training Prevention Professionals
Taken together, the three journeys demonstrate how MakSPH’s Environmental Health training converts diverse personal backgrounds into a shared professional orientation centred on prevention. Through interdisciplinary coursework, field placements, research mentorship, and leadership opportunities, students develop competencies that extend beyond technical knowledge to include systems thinking and public engagement.

The BEHS programme, established in 2000 within MakSPH’s Department of Disease Control and Environmental Health, remains the School’s only undergraduate degree and has trained more than 1,000 graduates who now serve across government institutions, non-governmental organisations, academia, and international health programmes. Its continued evolution reflects growing recognition that strengthening health systems requires professionals capable of addressing environmental risks before illness occurs.
The achievements of this year’s graduates, therefore, represent more than academic distinction. They reflect a model of training designed to prepare professionals whose work reduces the need for treatment by preventing disease at its source, reinforcing MakSPH’s role in shaping Uganda’s environmental health workforce.
Health
Philliph Acaye and the Making of Uganda’s Environmental Health Workforce
Published
1 week agoon
February 24, 2026
As Makerere University School of Public Health (MakSPH) presents 29 graduands on February 25, 2026, at Makerere University’s 76th Graduation Ceremony, for the conferment of the Bachelor of Environmental Health Science (BEHS) degree, the journey of the cohort’s best student provides a compelling window into both individual resilience and institutional impact. Philliph Acaye, graduating with a CGPA of 4.63, represents more than academic distinction. His story reflects the lived realities that shape many public health professionals in Uganda and shows how rigorous training can transform experience into leadership within health systems.

Education Shaped by Conflict
Acaye was born on October 2, 1993, in Wangduku Village, Palenga Parish, Pajule Sub-County, Pader District in northern Uganda, a region deeply affected by the Lord’s Resistance Army (LRA) insurgency in the early 2000s, where education and security often existed in constant tension. As a child, schooling unfolded alongside displacement and uncertainty, conditions that shaped an entire generation growing up during the conflict.
“Around 2002, before we had fully moved into the IDP camps, we often ran with our parents whenever there were LRA attacks,” he recalls. “But on several occasions, they caught us unaware. During one of the attacks, they abducted me and moved with me for close to seven kilometres, from Wangduku to Pajule Trading Centre in Pader. At first, they said I was too young to be moved with. I was around nine or ten years old. Later, I understood that someone among them personally knew my father and did not want me taken, so he used my age as the reason, and they left me behind.”

He narrates that several relatives and neighbours, including some of his childhood friends, were not spared, among them an uncle whose whereabouts remain unknown to this day. “If they had gone with me,” Acaye reflects quietly, “I could be dead, or I might not have studied.” The remark sits deep and places his graduation in context, not simply as personal success, but as the outcome of persistence through years when conflict repeatedly disrupted education across northern Uganda.
Between 2002 and 2006, his schooling continued inside Pajule Internally Displaced Persons (IDP) Camp, where families lived in overcrowded settlements and depended largely on relief food. Learning environments were unstable, teachers travelled under risk, and lessons were frequently interrupted by insecurity. Even within the camps, attacks remained possible. Education progressed slowly, but it continued, sustained by families and teachers who insisted that schooling remained essential despite uncertainty.
When communities gradually returned home, Acaye rebuilt his academic track record step by step. He completed Primary Leaving Examinations in 2007 with an aggregate of 19 and was the best pupil at Wangduku Primary School, at a time when enrolment remained low because many families feared returning to villages. He proceeded to Pajule Senior Secondary School, completing O-Level in 2011 with 31 aggregates, and later obtained 10 points at A-Level in 2013 from Kitgum High School.
However, his progression was shaped by consistent recovery after disruption, supported by relatives, teachers, community mentors, and educational assistance from Invisible Children, a post-LRA conflict recovery NGO led locally by Ms. Laker Jolly Okot, which supported his A-Level education.
Professional direction emerged during his training at the Mbale School of Hygiene, where he pursued a Diploma in Environmental Health Science from 2014 to 2016 and graduated with a strong CGPA of 4.4. The diploma opened immediate employment opportunities in community and humanitarian health settings back home, followed by service in local government. Today, he works as a Health Inspector in Kitgum District Local Government, implementing sanitation monitoring, infection prevention activities, and community health interventions. Practical experience strengthened his understanding of public health challenges but also revealed limits in technical depth that he felt required further training.
Training the Public Health Professional
His admission to MakSPH in 2022 through the government diploma-entry sponsorship scheme represented a deliberate academic decision rather than a career reset. He sought broader analytical skills and a stronger grounding in environmental health systems, particularly in areas of surveillance, planning, and evidence-based decision-making.
“I realised some technical aspects were not fully covered at the diploma level. I wanted to understand public health beyond implementation and learn how decisions are justified scientifically,” Acaye explained.

The sponsorship, he observed, transformed that ambition into possibility and remains central to how he understands his academic journey at Makerere University. “I am grateful to the Makerere University selection committee, the MakSPH selection committee, and the Government of Uganda for this opportunity. Opportunities like this are not guaranteed, and I recognise the trust placed in me to undertake and complete the three-year BEHS programme.”
The transition into university study was not seamless, though. His admission had come earlier than planned, and he began coursework without formal study leave while still tied to workplace obligations in Kitgum. Sustained support from district leadership, particularly Dr. Okello Henry Otto, the District Health Officer, eventually enabled him to secure study leave and concentrate fully on academic work. Now with stability came rapid academic improvement, supported by peer learning, faculty mentorship, and a strong curriculum that emphasised analytical reasoning alongside applied practice.
Acaye attributes his transformation to the programme’s academic culture rather than individual brilliance. “The programme helped me realise that what I was doing before was only a surface understanding,” he argued. “I learned to approach public health more deeply.” Exposure to research methods, he revealed, reshaped how he interpreted field experience and encouraged him to submit an abstract to an international academic conference, marking his transition from practitioner to emerging researcher.
For Mr. Abdallah Ali Halage, the MakSPH Coordinator of the BEHS programme, such outcomes reflect intentional design rather than coincidence. He noted that student success is rooted in a training philosophy that combines technical instruction with professional discipline from the moment students enter the programme. According to him, orientation focuses not only on coursework but also on expectations of conduct, independence, and responsibility. “When students join, we brief them on how seriously they must approach their academic journey,” he said. “That grounding helps shape their performance over time.”

Mr. Halage argued that while some high-performing students enter through diploma schemes, achievement ultimately depends on commitment and effort rather than background. He cited Acaye’s consistent curiosity and self-motivation as defining traits, noting that strong academic results tend to follow students who actively engage with the learning process.
“I congratulate Philliph and his colleagues upon attaining first-class honours and performing very well academically. Philliph has been hardworking and self-motivated. He has consistently shown a strong interest in his studies, and that commitment has helped him achieve this result. He has been a very good student,” Mr. Halage attested.
He added that the achievement reflects a broader culture within the programme. “Our students are disciplined and independent. Their commitment, together with support from the School management, the College and University leadership, has contributed greatly to their success.”

From Individual Achievement to Institutional Impact
The broader significance of Acaye’s achievement becomes clearer when placed within the evolution of the BEHS programme itself. Established in 2000 within MakSPH’s Department of Disease Control and Environmental Health (DCEH), the programme remains the School’s sole undergraduate degree and was among the earliest environmental health bachelor’s programmes in East Africa. In more than two decades, it has produced over 1,000 graduates, expanding professional capacity beyond diploma-level training and strengthening Uganda and the region’s environmental health workforce across government, non-governmental organisations, educational institutions, and points of entry such as airports and border services.
Mr. Halage explained that the programme helped redefine career pathways within the government of Uganda’s public service structures by introducing degree-level expertise into environmental health roles. Graduates now serve as Environmental Health Officers, Senior Environmental Health Officers, and technical specialists contributing to policy implementation and service delivery across multiple sectors. The academic pathway has also expanded vertically, with postgraduate training opportunities at MakSPH currently enabling graduates to progress into research, teaching, and doctoral-level specialisation, ensuring continuity within the discipline.

A Programme Shaping Regional Practice
The reputation of Makerere University’s Bachelor of Environmental Health Science programme is also increasingly influencing regional institutions. During a strategic benchmarking visit to MakSPH on July 30, 2025, Dr. Ratib Dricile, Dean of the Faculty of Health Sciences at Muni University, described the School of Public Health as a reference point for universities seeking to strengthen environmental health training in the region.
The main reason the delegation visited Makerere University School of Public Health was that Muni University remains a young and growing institution located in north-western Uganda along the borders with the Democratic Republic of Congo and South Sudan, where porous borders contribute to frequent cross-border diseases, many of which are preventable through strong environmental health approaches, Dr. Dricile explained.

“Makerere University, with over 100 years of institutional experience and 25 years running the Environmental Health programme, was the right place for us to benchmark, particularly in curriculum design, course content, programme structure, and implementation,” he said. “We were impressed by the work being implemented and gained more than we initially expected. By integrating these experiences, we believe the Muni University curriculum can become even stronger. The collaboration will allow us to adopt innovations built on Makerere’s long experience, and we believe that working together with Makerere University will strengthen Muni University institutionally and contribute positively to our university’s growth and ranking.”
It is within this institutional tradition, built over decades of training environmental health professionals across Uganda and the region, that Philliph Acaye’s achievement takes meaning. For him, graduating top of the class remains grounded in practical purpose rather than prestige. He views a first-class degree as an opportunity rather than an endpoint. Recalling guidance from his lecturers, he said strong academic results can open doors but must be followed by demonstrated competence. “A first class helps you get shortlisted,” he said. “After that, you must prove yourself.”

His immediate plans reflect that perspective. He is currently pursuing additional training in Health Services Management at Gulu College of Health Sciences while preparing for postgraduate study in either public health or environmental and occupational health. At the same time, he continues supporting pupils in his community and plans to mobilise resources to provide sanitary pads for girls at his former primary school, an initiative he believes will help reduce school dropout rates in rural areas.
Acaye’s journey, from disrupted schooling in an IDP camp to graduating top of MakSPH’s BEHS programme for the 2022 cohort, reflects the deeper purpose of public health education. As MakSPH presents its newest cohort for graduation this week, his story demonstrates how the programme turns lived experience into professional capacity, strengthening communities and health systems across Uganda and the region, one graduate at a time.
Health
Makerere University School of Public Health Graduates First Cohort of Cost-Effectiveness Analysis Short Course
Published
2 weeks agoon
February 20, 2026By
Mak Editor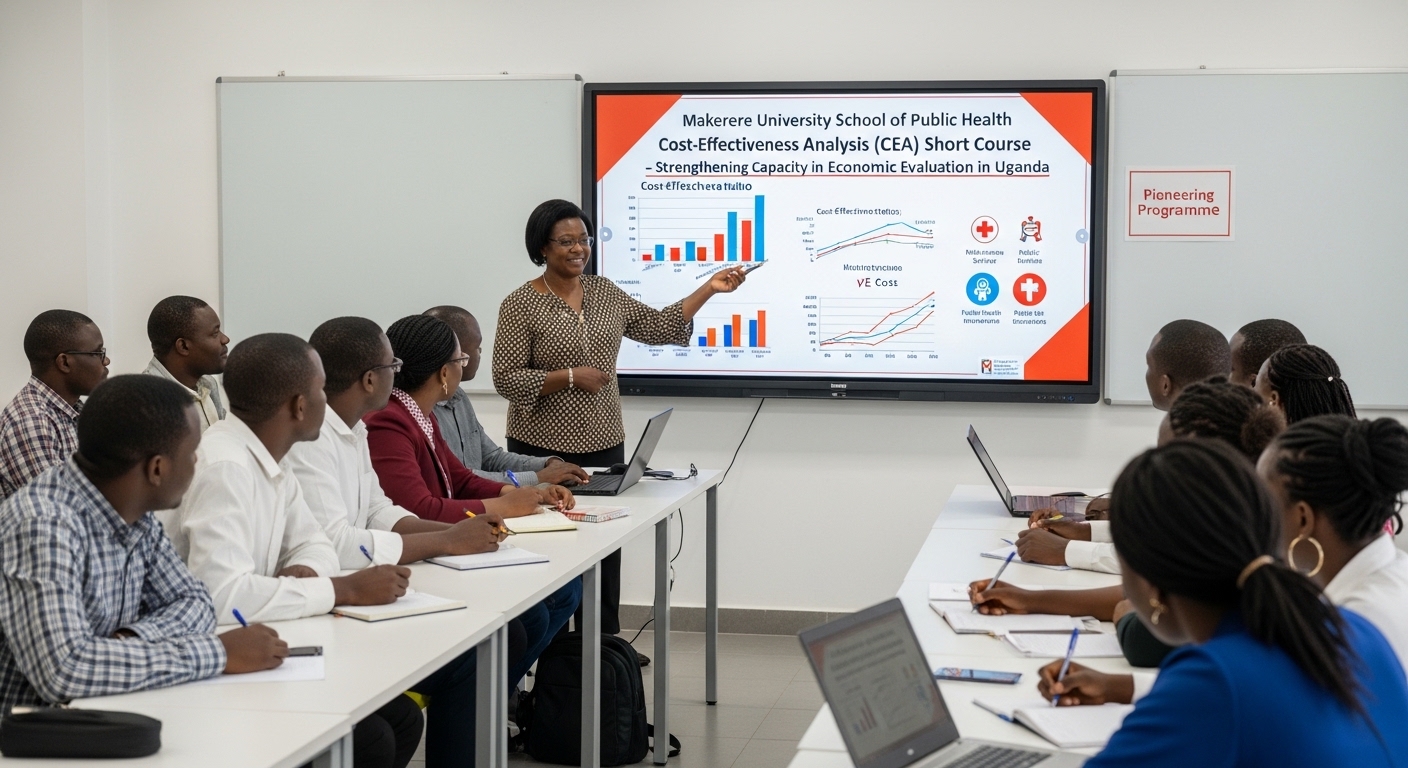
Kampala, Uganda – The Makerere University School of Public Health (MakSPH) has marked a significant milestone with the graduation of the first-ever cohort of its Cost-Effectiveness Analysis (CEA) Short Course. The pioneering programme is designed to strengthen capacity in economic evaluation in Uganda and beyond.
The virtual graduation ceremony honored eleven (11) participants who completed the course. The cohort included professionals from academia, research institutions, government agencies, and non-state actors, reflecting the increasing demand for skills in economic evaluation across sectors.
The short course was developed and implemented by the Department of Health Policy, Planning, and Management (HPPM) in response to the increasing need for evidence-informed decision-making in a context of limited resources.
In her remarks during the ceremony, Assoc. Prof. Suzanne Kiwanuka, Head of the Department of Health Policy, Planning and Management (HPPM) at MakSPH, congratulated the inaugural cohort for completing what she described as a “critical and timely” course.
“With decreasing resources and rising demand for services driven by population growth and the emergence of high-cost technologies, decision-makers must make difficult choices,” she noted. “Cost-effectiveness analysis is no longer optional. It is central to conversations in the corridors of power.”
The CEA short course was designed to equip policymakers, researchers, and practitioners with both theoretical knowledge and practical skills in economic evaluation. Participants were introduced to key principles of health economics, costing methodologies, decision-analytic modelling, Markov modelling, sensitivity analysis, and interpretation of incremental cost-effectiveness ratios (ICERs).
According to Prof. Elizabeth Ekirapa, the course lead at MakSPH, this inaugural offering had been “a long time coming,” following years of discussions within the department about building local expertise in economic evaluation.
Delivered over 10 days through interactive online sessions, the course combined lectures, case studies, and hands-on modelling exercises using contextually relevant datasets. Participants were required to develop and present applied cost-effectiveness projects as part of their assessment, allowing them to translate theory into practice.
During the feedback session at the graduation ceremony, faculty emphasized the importance of clarity in defining study perspectives, selecting appropriate outcomes, and aligning research questions with modelling approaches.
Dr. Chrispus Mayora, one of the facilitators, highlighted the need to carefully select outcomes that directly reflect the intervention being evaluated. “When thinking about outcomes, ask yourself: Is this aligned with what I want to study? Interesting outcomes are not always the most appropriate ones,” he advised.
Participants were also encouraged to select modelling techniques such as decision trees or Markov models based on the research question and the nature of the disease or intervention under study.
Prof. Ekirapa described the graduates as “trailblazers,” noting that their feedback would shape future iterations of the course. “When you are the first cohort, you are like pioneers,” she remarked. “We are committed to improving this course to ensure it becomes a world-class programme.”
For many attendees, the graduation ceremony was a new experience, as certificates were awarded virtually an approach that participants welcomed as innovative and inclusive.
“Cost-effectiveness analysis enables us to maximise value for money,” noted Dr. Crispus Mayora of MakSPH. “It allows decision-makers to compare interventions systematically and ensure that limited resources achieve the greatest possible benefit.”
The programme aligns with Makerere University’s broader mandate to provide high-quality training that responds to national and regional development priorities. Participants who successfully complete the course receive a certificate signed by the Dean of the School of Public Health.
As the ceremony concluded, faculty encouraged continued engagement beyond the classroom. Graduates were urged to refine their project ideas and collaborate with the department in advancing research and policy discussions.
The successful completion of the first CEA short course marks an important step in building a cadre of professionals equipped to conduct rigorous economic evaluations. With plans to expand and refine the programme based on participant feedback, the HPPM department under MakSPH is positioning itself as a regional leader in health economics and policy analysis training.
Trending
-

 Humanities & Social Sciences1 week ago
Humanities & Social Sciences1 week agoMeet Najjuka Whitney, The Girl Who Missed Law and Found Her Voice
-

 General1 week ago
General1 week ago76th Graduation Highlights
-

 Health2 weeks ago
Health2 weeks agoUganda has until 2030 to end Open Defecation as Ntaro’s PhD Examines Kabale’s Progress
-

 Agriculture & Environment2 weeks ago
Agriculture & Environment2 weeks agoUganda Martyrs Namugongo Students Turn Organic Waste into Soap in an Innovative School Project on Sustainable Waste Management
-

 General2 weeks ago
General2 weeks agoMastercard Foundation Scholars embrace and honour their rich cultural diversity
