Health
Makerere University Launches Social Innovation in Health Initiative Community of Practice
Published
10 months agoon

Kampala, 09 April 2025— Makerere University has officially launched the Social Innovation in Health Initiative Community of Practice (SIHICOP)—a new platform designed to connect local health innovators with policymakers, donors, and researchers. The goal: to turn scattered success stories into a powerful, nationwide movement that reimagines healthcare from the ground up.
The launch, held during the 6th National Social Innovation in Health Stakeholders’ Workshop at Hotel Africana in Kampala, drew a dynamic mix of changemakers, health innovators, academics, donors, and government leaders, all rallying around one idea: that equitable, sustainable healthcare must be rooted in communities.
While Uganda has made notable progress, cutting under-five deaths by 66% since 2000, challenges remain. Fifty out of every 1,000 children still die before their fifth birthday. Nearly half suffer from stunting due to malnutrition. In rural areas, pregnant women walk for hours to reach clinics. Across the country, hospitals battle frequent drug shortages.
Dr. Phyllis Awor, Director of the SIHI Uganda Hub at Makerere University’s School of Public Health (MakSPH), emphasized the critical role of social innovation in closing healthcare gaps. “Half of Ugandan children lack basic vaccinations, and 40% face stunting. These challenges demand creative, inclusive solutions co-created with communities,” she said.
“We’ve spent a decade identifying, studying, and strengthening grassroots innovations. Through our six-month fellowship program, we train innovators in monitoring and evaluation, research, communication, impact assessment, and fundraising so their work doesn’t just survive but scales,” she said. “Today, we’re awarding them completion certificates and launching them into a vibrant community of practice.”
Dr. Awor, who is also a Lecturer and Researcher maintains Social Innovation is about solving these real problems with real people. With the support of the Swedish Embassy and the World Health Organization’s TDR program, SIHICOP, she says, will foster peer learning, capacity-building, and scaling of innovations like mobile health platforms and community-based maternal care.

Since 2017, Uganda’s SIHI hub has supported 30 homegrown innovations, impacting tens of thousands of lives. “We’ve identified 21 standout solutions so far,” Dr. Awor shared. “But if we want them to go national, we need enabling policies.”
Globally, SIHI was founded in 2014 to bring together innovators, communities, policymakers, and academics across the Global South. With 15 hubs, including Uganda’s, SIHI has documented over 200 innovations and 40 case studies that demonstrate the power of grassroots solutions to improve health systems.
Dr. Olaro Charles, Uganda’s Acting Director General of Health Services, acknowledged that bureaucracy often stifles good ideas. “Sometimes, a small change in how you look at a problem can produce the best and most marketable solution,” he said.
He spoke from experience. As a clinician, Dr. Olaro led efforts to curb drug theft and stockouts by tightening distribution and boosting accountability. “It’s not like people walk off with whole boxes,” he explained. “But if you have 300 employees and each takes just one dose… that adds up. We introduced medicine returns, round-the-clock pharmacies, and ward-level audits. At first, there was resistance, but it worked.”
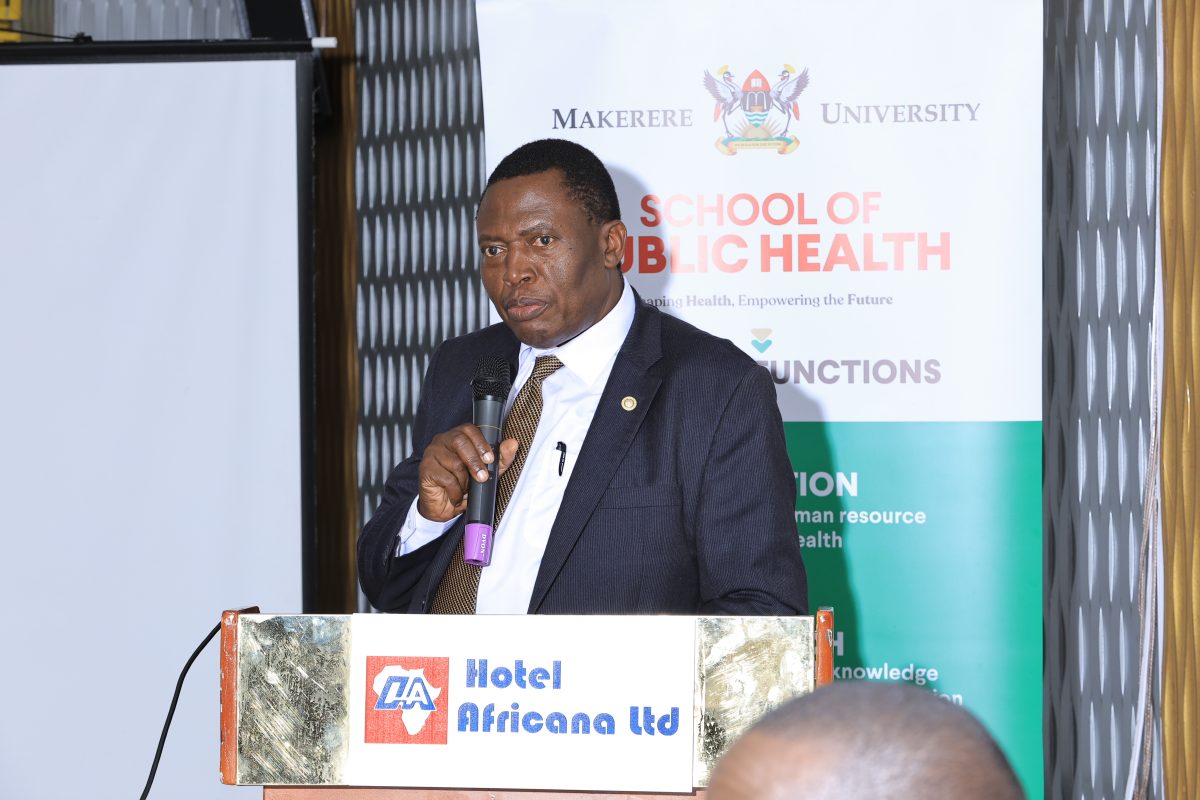
Another one of his most memorable innovations was setting up a neonatal unit for premature babies while he was a Medical Superintendent. “I remember a baby who weighed less than a kilo, barely six months old, and survived. We pushed survival rates to 85%. Eventually, we ran out of space. We began asking ourselves: Where had these children been going before? Previously, these children may have died within the community. These are innovations that create real, tangible impact. And I’m sure many of the things you’re doing here are creating similar results.”
He urged the Fellows to treat their innovations like living systems: “If they survive infant mortality, they’ll live longer. These ideas deserve to grow.”
Mr. Tomas Lundström, Health Counsellor at the Swedish Embassy, spoke with deep conviction about Sweden’s long-standing investment in Uganda’s future. “For decades, Sweden has believed in Uganda’s greatest asset, its people,” he said. “Through Sida, we funded the training of over 500 Makerere staff for PhDs. I didn’t start it. I didn’t train your PhDs. The Swedish taxpayers actually funded the training. Now that wasn’t just investment; it was transformation. It’s one reason Makerere is the powerhouse it is today.”
Lundström also shared a memory that continues to shape his view of development. While inspecting UNICEF projects in Zambia in 1998, he recalled visiting five villages where only one had shown some success. A driver suggested they visit the last village, the 5th. “We went. No one was there. We waited, then a man came running, covered in dirt. He was the village chief,” Lundström recounted. “He said something I’ve never forgotten: ‘Thomas, when the rainy season comes, we can’t take pregnant women to the clinic. Do you know where I can learn to build a bridge’?”

“That was different from what I usually hear—‘Can we have some money?’ Real change doesn’t come from handouts. It starts within communities.”
But Lundström warned that international aid is under strain. “We’ve already lost a lot of funding from U.S. and other donors. Ukraine, Sudan—global crises are pulling resources away. We must get creative. We must find new ways to secure resources.”
Still, he was optimistic. “We’re seriously considering continued support for another year. We’re also pushing for deeper collaboration between Makerere and Karolinska Institutet. But it’s up to you too,” he said.
He praised Dr. Phyllis Awor and her team: “What sets them apart is not just competence, but passion. She doesn’t do this because it’s her job; she does it because she believes in it. Because everyone deserves a fair chance, a seat at the table, a bit of hope.”
Makerere University Vice Chancellor, Professor Barnabas Nawangwe, echoed those sentiments, describing the School of Public Health as the university’s “engine of change.” He noted that the School contributes to nearly 30% of all university publications—and brings in 40% of its research funding.
“That’s no accident,” he said. “Public health is critical. Without health, there is no progress. That’s why donors invest in public health issues.”

He described the social innovation initiative as a model for how academia and communities can work together, not just to publish but to transform lives. “When global rankings name Makerere the most community-impactful university, they’re recognizing what happens when scholars step beyond lecture halls. This is what happens when researchers dig deep into the ground to cultivate solutions that transcend national boundaries.
The Vice Chancellor also paid tribute to Sweden’s role in that transformation. “We cannot thank the people of Sweden enough. Their support through Sida trained over 500 of our staff to the PhD level—the largest staff development initiative I’ve seen at any university, anywhere. It came when we needed it most, after the war. That’s why Makerere stands today as a leading research institution in Africa.”
He congratulated the 2024/25 Fellows, praising their inspiring journeys, and commended Dr. Awor and her remarkable team of researchers for achieving what only world-class institutions can: “melding razor-sharp academia with the wisdom of villages, policy muscle with frontline innovations.”

You may like
-


Makerere Launches Scholarly Guide, Calls for Increased Research, Publication and Innovation in Africa
-


BOKU University Charts New Collaboration Strategies with Mak’s Department of Zoology, Entomology & Fisheries Sciences
-


When Birth Becomes the Most Dangerous Moment, Wanduru & the Work of Making Labour Safer
-


Study Alert: Power in Her Hands; Why Self-Injectable Contraception May Be a Game Changer for Women’s Agency in Uganda
-


Building Skills for Better Public Investments: PIM Centre Trains Public Sector Economists
-


How Jimmy Osuret Turned Childhood Trauma into Evidence for Safer School Crossings
Health
Call for Applications: Short Course in Molecular Diagnostics March 2026
Published
5 days agoon
February 12, 2026By
Mak Editor
Makerere University College of Health Sciences, Department of Immunology and Molecular Biology, in collaboration with the Makerere University Biomedical Research Centre (MakBRC), is pleased to invite applications for a Short Course in Molecular Diagnostics scheduled for 23rd–27th March 2026.
This hands-on course will introduce participants to core principles and practical skills in molecular diagnostics, including nucleic acid structure and function, laboratory design and workflow, PCR setup, gel electrophoresis and DNA band interpretation, contamination control and quality assurance, and clinical applications of PCR in disease diagnosis.
The training will take place at the Genomics, Molecular, and Immunology Laboratories and will accommodate 30 trainees. The course fee is UGX 500,000.
Target participants include:
- Graduate students with basic exposure to molecular biology (e.g., MICM, MSBT)
- Final year undergraduate students (e.g., BBLT, BMLS)
- Medical and veterinary clinicians
- Agricultural professionals interested in practical molecular biology
To apply, please send your signed application via email to nalwaddageraldine@gmail.com (copy Dr. Eric Kataginy at kataginyeric@gmail.com). Indicate your current qualification, physical address, and phone contact (WhatsApp preferred), and attach a copy of your National ID or passport data page, your current transcript or testimonial, and your degree certificate (if applicable).
The application deadline is 13th March 2026. Successful applicants will be notified by email. Admitted participants are required to pay the course fee within five days to confirm their slot.
For further inquiries, don’t hesitate to get in touch with Ms. Geraldine Nalwadda on +256 701 361449.
See download below for detailed call.
Health
When Birth Becomes the Most Dangerous Moment, Wanduru & the Work of Making Labour Safer
Published
6 days agoon
February 11, 2026
The ward is never quiet during labour. Even at night, there are cries, some sharp with pain, others muted by exhaustion. Monitors beep. Midwives move quickly between beds. In the moments just before birth, everything narrows to breath, pressure, and time.
It was in places like this, years ago, that Phillip Wanduru first learned how fragile that moment can be.
Working as a clinical nurse at Nakaseke Hospital in central Uganda, he watched babies who should have survived struggle for breath. Some were born still. Others cried briefly, then went silent. Many were not premature or unusually small; they were full-term babies whose lives unraveled during labour.
“What troubled me most,” Wanduru recalls, “was that these were complications we have known how to manage for more than a hundred years, prolonged labour, obstructed labour, and hypertension. And yet babies were still dying or surviving with brain injuries.”
Those early encounters never left him. They became the questions that followed him into public health, into research, and eventually into a doctoral thesis that would confront one of Uganda’s most persistent and preventable tragedies.

A Public Defense, Years in the Making
On Friday, June 13, 2025, Wanduru stood before colleagues, mentors, and examiners in a hybrid doctoral defense held at the David Widerström Building in Solna, Sweden, and online from Kampala. The room was formal, but the subject matter was anything but abstract.
His PhD thesis, “Intrapartum-Related Adverse Perinatal Outcomes: Burden, Consequences, and Models of Care from Studies in Eastern Uganda,” was the culmination of years spent listening to mothers, following newborns long after delivery, and documenting what happens when birth goes wrong.
He completed the PhD through a collaborative programme between Makerere University and Karolinska Institutet, under the supervision of Prof. Claudia Hanson, Assoc. Prof. Peter Waiswa, Assoc. Prof. Helle Mölsted Alvesson, and Assoc. Prof. Angelina Kakooza-Mwesige, a team that bridged global expertise and local reality. His doctoral training unfolded as the two institutions marked 25 years of collaboration, a partnership that has shaped generations of public health researchers and strengthened research capacity across Uganda and beyond.
By the time he defended, the findings were already unsettlingly clear.

One in Ten Births
In hospitals in Eastern Uganda, Wanduru’s research found that more than one in ten babies experiences an intrapartum-related adverse outcome. This medical term refers to babies who are born still, die shortly after birth, or survive with brain injury caused by oxygen deprivation during labour.
Among those outcomes, stillbirths accounted for four in ten cases. Five in ten babies survived with brain injury.
“These are not rare events,” Wanduru explains. “They are happening every day, often in facilities where care should be available.”
But survival was only part of the story.
Following infants diagnosed with intrapartum-related neonatal encephalopathy for a year, his research revealed that about seven in ten babies with severe brain injury died before their first birthday. Among survivors, many faced lifelong challenges, difficulty walking, talking, and learning.
“What happens in labour,” he says, “does not end in the delivery room. It follows families for years.”
He describes the findings of his PhD research as appalling, evidence of an urgent failure in how labour and delivery are managed, and a call for immediate action to prevent avoidable complications. “Babies with severe brain injuries,” he notes, “faced the greatest odds. Even when they survived birth, nearly seven in ten died before their first birthday. Of those who lived beyond infancy, about half were left with long-term challenges, including difficulties with walking, talking, or learning.”

Mothers at the Centre—Yet Often Invisible
Wanduru’s work did not stop at numbers. Through in-depth interviews with mothers and health workers, he uncovered a quieter truth that parents, especially mothers, were desperate to help their babies survive, but often felt unsupported themselves.
Mothers followed instructions closely. They learned to feed fragile babies, keep them warm, and monitor breathing. They complied with every rule, driven by fear and hope in equal measure.
“The survival of the baby became the only focus,” Wanduru says. “But the mothers were exhausted, emotionally drained, and often ignored once the baby became the patient.”
Even as mothers remained central to care, their own physical and mental well-being received little attention. For the poorest families, the burden was heavier still: long hospital stays, transport costs, and uncertainty about the future.
These insights shaped one of the thesis’s most powerful conclusions: saving newborn lives requires caring for families, not just treating conditions.
Why Care Fails—Even When Knowledge Exists
One of the most uncomfortable findings in Wanduru’s research was that emergency referrals and caesarean sections did not consistently reduce the risk of brain injury, except in cases of prolonged or obstructed labour.
The problem, he found, was not the intervention, but the delay.
In many facilities, hours passed between identifying a complication and acting on it. Ambulances were unavailable. Referral systems were weak. Operating theatres lacked supplies or staff.
“These are not failures of science,” Wanduru says. “They are failures of systems.”
His work reinforces a sobering reality for policymakers that most intrapartum-related deaths and disabilities are preventable, but only if care is timely, coordinated, and adequately resourced.
From Bedside to Systems Thinking
Wanduru’s path into public health began at the bedside. After earning a Bachelor of Science in Nursing from Mbarara University of Science and Technology in 2011, he trained as a clinician, caring for patients during some of their most vulnerable moments. He later completed a Master of Public Health at Makerere University in 2015, a transition that gradually widened his focus from individual patients to the health systems responsible for their care.
His work gradually drew him deeper into the systems shaping maternal and newborn care. As a field coordinator for the MANeSCALE project, he worked within public and private not-for-profit hospitals, helping to improve clinical outcomes for mothers and babies. Under the Preterm Birth Initiative, he served as an analyst, contributing to efforts to reduce preterm births and improve survival among vulnerable infants through quality-improvement and discovery research across Uganda, Kenya, and Rwanda.
In the Busoga region, he coordinated prospective preterm birth phenotyping, following mothers and babies over time to better understand the causes and consequences of early birth. Since 2016, this work has been anchored at Makerere University School of Public Health, where he serves as a Research Associate in the Department of Health Policy, Planning, and Management.
Across these roles, he found himself returning to the same question: why babies continue to die during a moment medicine has long learned to handle.
Models of Care That Could Change Outcomes
Wanduru’s thesis does more than document failure; it points toward solutions.
He highlights family-centred care models, including Kangaroo Mother Care, which keep babies and parents together and improve recovery, bonding, and brain development. He emphasizes early detection of labour complications, functional referral systems, and rapid access to emergency obstetric care.
“These are not new ideas,” he says. “The challenge is doing them consistently.”
He also calls for recognizing stillbirths, not as inevitable losses, but as preventable events deserving data, policy attention, and bereavement support.
“Stillbirths are often invisible,” he notes. “But they matter to mothers, to families, and to the health system.”
Research That Changes Practice
For Wanduru, the most meaningful part of the PhD journey is that the evidence is already being used. Findings from his work have informed hospital practices, advocacy reports, and quality-improvement discussions.
“Yes, the PhD was demanding,” he admits. “But knowing that the work is already contributing to change makes it worthwhile.”
His mentors see him as part of a broader lineage, researchers committed not only to generating evidence but to ensuring it improves care.
With a PhD in his bag, Wanduru sees his work as a continuation rather than a conclusion.

“The fight to make birth safe for every mother and baby continues,” he says. “I want to contribute to improving care and to building the capacity of others to do the same.”
That means mentoring young researchers, strengthening hospital systems, and keeping the focus on families whose lives are shaped in the delivery room.
Dr. Wanduru joins fellows in the MakSPH PhD forum who concluded their doctoral journeys in 2025, and his work speaks for babies who never cried, for mothers who waited too long for help, and for health workers doing their best within strained systems. It insists that birth, while always risky, does not have to be deadly.
— Makerere University School of Public Health Communications Office, Graduation Profiles Series, 76th Graduation Ceremony
Health
Study Alert: Power in Her Hands; Why Self-Injectable Contraception May Be a Game Changer for Women’s Agency in Uganda
Published
7 days agoon
February 10, 2026By
Mak Editor
By Joseph Odoi
In the remote villages of Eastern and Northern Uganda, a small medical device is doing far more than preventing unintended pregnancies, it appears to be quietly shifting the balance of power in women’s lives.
A new study titled “Is choosing self-injectable contraception associated with enhanced contraceptive agency? Findings from a 12-month cohort study in Uganda” has revealed that self-injection gives women more than just a health service, it can boost their confidence, control, and agency over their reproductive health.
The research was conducted by Makerere University namely; Professor Peter Waiswa, Catherine Birabwa, Ronald Wasswa, Dinah Amongin and Sharon Alum in collaboration with colleagues from the University of California, San Francisco
Why this Study matters for Uganda
For decades, family planning in Uganda has followed a provider-client model. Women travel long distances to clinics, wait in queues, and rely on health workers to administer contraception. This system creates barriers transport costs, clinic stock-outs, long waiting times, and limited privacy.
Self-injectable contraception, known as DMPA-SC, disrupts this model by shifting care from the clinic to the individual woman.
DMPA-SC is a discreet, easy-to-use injectable that women can administer themselves after receiving basic training and counselling.
What the Data Tells Us
To see if self-care technology actually shifts the needle on women’s power, researchers tracked 1,828 women across Eastern (Iganga and Mayuge Districts) and Northern Uganda (Kole, Lira, and Oyam Districts) for a full year. They compared women who chose to self-inject their birth control (216 women) against a control group, most of whom chose methods requiring dependency on clinics (1,612 women).
The Six-Month “Agency Spike”
The study used a Contraceptive Agency scale (scored from 0 to 3) to measure a woman’s internal confidence and her ability to act on her health choices.
The Self-Injectors
For the Self Injectors, their agency scores rose significantly, from 2.65 to 2.74 by the six-month mark.
The Clinic-Dependent Group
Scores for the group using mostly provider-led methods (like clinic shots or implants) remained nearly flat, moving from 2.61 to only 2.63.
Within just six months, women who took control of their own injections noted that they felt a measurable boost in their Consciousness of reproductive Rights (0.08 points) since they transitioned from being passive recipients of care to active decision-makers.
Using the Agency in Contraceptive Decisions Scale (scored 0–3), the study found a clear empowerment advantage for women who chose self-injection.
The findings come at a time when Uganda has reaffirmed its commitments under FP2030, aiming to expand access to voluntary, rights-based family planning. The study also aligns with the National Family Planning Costed Implementation Plan, which prioritises method choice, equity, and continuation, as well as national gender and youth empowerment strategies.
Can Uganda Sustain and Scale DMPA-SC?
Self-injectable contraception does not require continuous high-cost investment. Training and rollout costs are largely one-time, and the main recurring expense is the contraceptive commodity itself. Compared with the cumulative costs of repeated clinic visits for both the health system and women self-injection is more cost-effective over time.
Advancing primary health care with DMPA-SC
Beyond cost savings, self-injection eases pressure on health facilities and allows health workers to focus on more complex care. It also extends health services into communities, supporting continuity of care in areas where facilities are few and far between. In this way, family planning is no longer confined to the clinic.
While donor support has helped introduce the method, it can be sustained locally without relying on external funding. “With predictable national financing and reliable commodity supply chains, DMPA-SC can reach more women and be fully integrated into Uganda’s health system, strengthening both access and community-level service delivery’’ according to the researchers.
Implications for Policy and Practice
As Uganda continues to reform its primary health care system, the findings add evidence to ongoing discussions about how family planning services are delivered, financed, and prioritised.
The research also positions self-injectable contraception not as a temporary innovation, but as a scalable method with the potential to be embedded within national systems provided that commodity availability and financing are safeguarded.
To ensure these gains are lasting, researchers recommend moving beyond the technology and addressing the structural and social barriers that can limit women’s agency.
Key recommendations from the researchers include the following
1. Reliable Supply Chains
Empowerment collapses when products are unavailable. DMPA-SC must be consistently stocked at the community level.
2. Creating a Supportive Social Environment
Privacy concerns, stigma, and partner resistance must be tackled through community engagement and sensitisation.
3. Prioritizing Informed Choice
Self-injection should be offered as a top-tier option in every facility, framed as a fundamental right to autonomy rather than just a medical convenience.
4. Integrated Counseling
Providers must be trained to support women not only in the “how to inject” but also in navigating the social challenges of self-care.
On the next step, the researchers call for a clear integration of DMPA-SC into national health financing, protection of family planning commodity budgets, and deliberate scaling of self-injectable contraception within Primary Health Care reforms. These actions will ensure sustainability, reliable access, and greater control for women over their reproductive choices according to the researchers.
Read the full study here: https://www.contraceptionjournal.org/article/S0010-7824(26)00003-X/fulltext
Trending
-

 General2 weeks ago
General2 weeks agoCall for Applications: Admission to Postgraduate Programmes 2026/2027
-

 Natural Sciences2 weeks ago
Natural Sciences2 weeks agoSimon Mungudit: Mak’s Best Performing Male Science Student & Rising Star in Petroleum Geoscience
-

 Agriculture & Environment2 weeks ago
Agriculture & Environment2 weeks agoFrom Adversity to Excellence: The Inspiring Journey of Makerere’s Best Science Student, Esther Ziribaggwa
-

 General7 days ago
General7 days agoAptitude Exam (Paper 1) Results for the Mature Age Entry Scheme 2026/2027
-
 Health2 weeks ago
Health2 weeks agoEU Earmarks Shs19.8bn for 15 Joint PhD Scholarships in Health, Environment Research
