Health
Mak Launches Homegrown COVID-19 Rapid Antibody Test Kits
Published
4 years agoon

By: Harriet Adong, Mak-RIF Communications Officer
The afternoon of Wednesday March 17th, 2021 saw Makerere University’s Department of Immunology and Molecular Biology, College of Health Sciences (CHS) launch the homegrown COVID-19 Rapid Antibody Test Kits. The COVID-19 Rapid Antibody Test Kits developed domestically aim to address challenges related to affordability/cost using imported items, promote research and innovation in the medical/health field and Makerere University in general.
This project was spearheaded by Dr. Misaki Wayengera, Director Biomedical Research at the Department of Immunology and Molecular Biology, College of Health Sciences, Makerere University. Dr. Wayengera is also the Chairperson of the Scientific Advisory Committee on the COVID-19 Taskforce in the Ministry of Health. These efforts are directed towards enhancing the fight against the spread of the Corona Virus not only at Makerere University but also in the entire country. Explaining the advantages of the project, Dr. Wayengera said “Makerere University has developed an affordable (costing less than US $1), easy to use (requiring minimal expertise, user guide), rapid (yielding results within 2-5 minutes) point of care test platform for COVID-19 suited for use within remote equatorial African settings. This will enable rapid testing for Coronavirus and considerably lower the cost of testing currently standing at USD 65, which is prohibitive for developing countries like Uganda. This could not have been achieved without the financial support of Partners and Institutions such as Supervised Financial Institutions under their umbrella body Uganda Bankers Association, Deposit Protection Fund of Uganda, and Government of the Republic of Uganda, the French Embassy in Uganda and Uganda’s Ministry of Science Technology and Innovation’’.
The Test Kit involves using a swab-tube dipstick to do an antigen test by use of a nasal sample. With this quick test, once the nasopharyngeal sample is obtained, it is placed back into its tube containing reagents that detect the virus surface protein.

This event was attended by Uganda’s Minister of Health; Hon. Dr. Jane Ruth Aceng Ocero, Uganda’s Minister of Science Technology and Innovation; Hon. Dr. Elioda Tumwesigye, French Ambassador to Uganda; His Excellency Jules-Armand Aniambossou, the World Health Organization Country Representative; Dr. Yonas W. Tegeny, Uganda’s Director General at Ministry of Health; Dr. Henry Mwebesa and the Permanent Secretary at Ministry of Health; Dr. Diana Atwine. The funders were also represented at the event and these included; Makerere University Research and Innovations Fund (Mak-RIF) represented by Dr. Roy William Mayega, Mak-RIF Coordinator, Uganda Bankers Association represented by Mr. Wilbrod Owor, the French Embassy and Ministry of Science Technology and Innovation like earlier listed among other dignitaries.
At the occasion, Prof. Damalie Nakanjako, Principal Makerere University College of Health Sciences represented Makerere University’s Vice Chancellor Prof. Barnabas Nawangwe. She welcomed all scientists, innovators and the media fraternity (representing the community) to witness yet another stride in and by faculty in Uganda’s leading higher institution of learning-Makerere University. In her remarks, she noted that, the University has through College of Health Sciences built extensive expertise, experience and eco-systems across the academia and partnerships for Research and Development of pathogen diagnostic. “This kit will carry out antibody tests. It will also be used in early detection of COVID-19 cases, used in screening of travelers for COVID-19, detection of symptoms as well as aid in sero-prevalennce studies to determine previous exposure to COVID-19. Makerere University is hopeful that this will enable Uganda and other African countries to cost-effectively respond to the COVID-19 pandemic”.
Makerere University is grateful for the SEED funding (UGX 65, 527, 020) from the Government of the Republic of Uganda through Makerere University Research and Innovations Fund (Mak-RIF) which aided initialization of this project. The Government of the Republic of Uganda is funding cross disciplinary research and innovations (over 500 projects now, up to a tune of Uganda Shillings 60 billion only for the last two financial years). Makerere University faculty and students have through this initiative engaged with other institutions, organizations, disciplines and Ministries enhancing research and innovations in and outside the institution. For all this support, we are truly grateful to the Government of the Republic of Uganda and all our other funders/partners, Prof. Nakanjako added.

Hon. Dr. Elioda Tuwesigye, Minister of Science Technology and Innovation in Uganda noted that such strides like the launch of Makerere University homegrown COVID-19 Rapid Antibody Test Kits was only a wake-up call to all of us that the virus is still with us and we can together do so much to up the fight against further spread and effects. He thanked the Government of the Republic of Uganda for funding research and innovations in Makerere University and other institutions too. “It is through research that we garner additional knowledge to enable us to be and remain creative. Embracing Research and Innovation is the way to go if we are to realize development in our country, Africa and the globe’’, he added.
Uganda’s Minister of Health at the event in her remarks congratulated all scientists at Makerere University including Dr. Wayengera and his research for working closely with the Ministry to respond to diverse community challenges and in this case the Coronavirus. She noted that this virus is still with us and thus the need for us to continue observing the Standard Operating Procedures, researching ad innovating to carry on with the fight. She added that some countries were experiencing the second and third wave of Coronavirus and thus Ugandans must remain on the alert regardless of the circumstances at the moment so that these waves do not crop in and sweep away the population. Hon. Dr. Aceng said: “These rapid antibody testing kits come at a point when we are preparing for the next wave of the COVID-19 pandemic, thank you Dr. Wayengera and team.’’
His Excellency Jules-Armand Aniambossou, French Ambassador in his remarks noted that the French Embassy in Uganda was and is happy to collaborate with and further support Makerere University’s efforts to respond to the Coronavirus. He said “Uganda’s response to COVID-19 was and is strong, immediate ad efficient. We need to learn from Uganda. Uganda can compete globally. Well done Scientists, he said as he officially launched the homegrown COVID-19 Rapid antibody Test Kits’’.
In the drive to raise funds towards the fight against the COVID-19 pandemic, and in response to Government’s call for support to join hands, Members of Uganda Bankers Association (UBA) and the Deposit Protection Fund contributed UGX. 200million to the project which was in advanced stages in 2020. Speaking at the occasion, Mr. Wilbrod Owor-Executive Director UBA applauded Makerere University for the research efforts as an academic institution and the quick turnaround invention. “The pandemic has had diverse effects on the economy and one of the most affected sectors are education, tourism & hospitality, real estate which ultimately have affected the banking sector by way of increase in Non-Performing Loans. In addition to the loan restructures that member banks have offered, as part of support to business community, we are also happy to have invested to support testing. Therefore, the affordability of this intervention is much welcome to address cost issues that would otherwise have to be so high for an average Ugandan” Owor said.
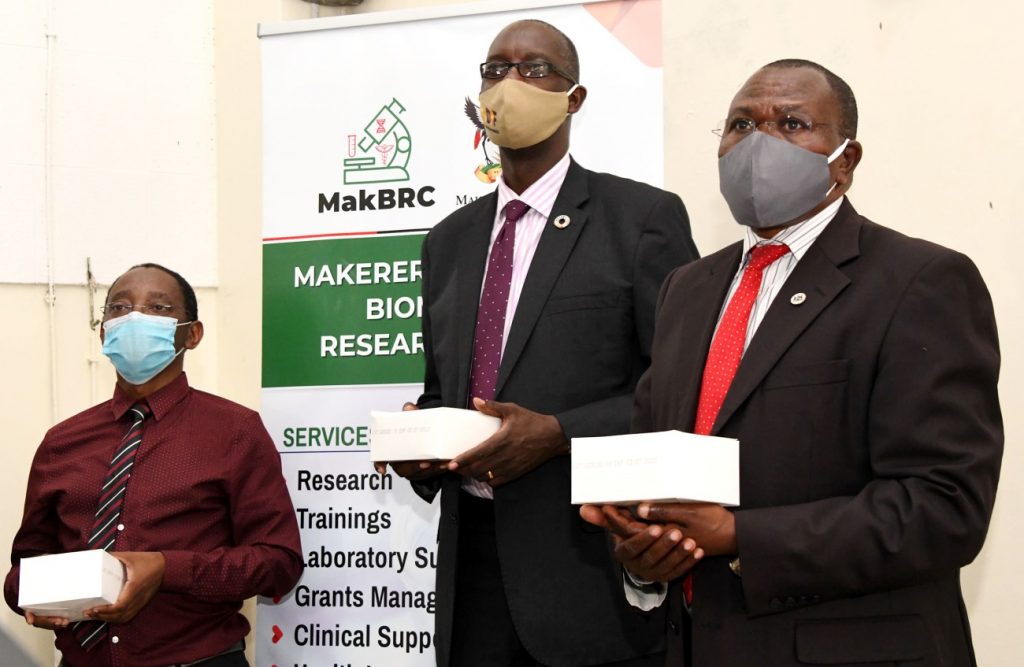
Dr. Roy William Mayega, Coordinator at the Makerere University Research and Innovations Fund (Mak-RIF) on behalf of Prof. William Bazeyo, Chair Mak-RIF thanked Dr. Wayengera and his research/innovation team for the work well done. He also thanked all funders for positively responding to the call for more resources to realize this project. He said “It is only when funders see such research and innovation outputs like the COVID-19 Rapid antibody Test Kits we are holding in our hands now that they will look further into their Bank Accounts to raise more resources to further support research and innovations. Thank you Dr. Wayengera and all the other Scientists for leading by doing. Let us continue with these efforts’’.
Dr. Wayengera acknowledged all the support/funding and gave each donor a pack of the COVID-19 Rapid Antibody Testing Kits.

The event host, Prof. Nakanjako, Principal at Makerere University’s College of Health Sciences then thanked all participants and welcomed them to further engage in a cocktail as volunteers led by the Director General and Minister of Health experienced antibody testing using the newly launched kits. The rest of the COVID-19 Test Kits will be used in the Makerere University Medical School laboratories
Congratulations Makerere University and congratulations the Government of the Republic of Uganda!
‘We Build for the Future, For God and My Country’
View and read about this launch in the Media
- New COVID-19 rapid antibody test kits launched to reduce cost and promote research. – https://joripress.com/new-covid-19-rapid-antibody-test-kits-launched-to-reduce-cost-and-promote-research
- https://www.ntv.co.ug/ug/news/national/local-testing-ability-improves-with-new-covid-19-kits-3326454
- https://chimpreports.com/makerere-launches-own-covid19-testing-kit/
- https://www.independent.co.ug/makerere-university-launches-covid-19-anti-body-test-kits/
- https://twitter.com/JaneRuth_Aceng/status/1372187357781360642?s=1002
- https://www.monitor.co.ug/uganda/news/national/scientists-behind-uganda-s-first-coronavirus-test-kits-3327390
- New Vision Newspaper Friday March 19th , 2021, Page 10
- Daily Monitor Newspaper Thursday March 18th , 2021 Page 6
You may like
-

Simplicity, Service & Scholarship: Hallmarks of Professor Livingstone Luboobi’s Legacy
-


Strengthening Grants Management Through Institutional Collaboration and Capacity Building
-


Mak Moves to Revitalize Food Technology & Business Incubation Centre to Drive Innovation & Entrepreneurship
-


Advert: Postgraduate Admissions 2025/26
-

Ugandan Study Flags Girls and Senior Students as a Mental Health High-Risk Group
-


Call for Applications: Responsible Conduct of Research (RCR) Training Course
General
Strengthening Grants Management Through Institutional Collaboration and Capacity Building
Published
4 days agoon
July 15, 2025
As the funding to the higher education sector keeps on reducing due to competing priorities, universities are implored to come up with structures and strategies to attract and win research grants.
Key findings indicate that universities with institutionalized grant management offices, strong and coordinated research teams are better positioned to effectively compete for grants.
Makerere University, in partnership with Northwestern University, is spearheading the E-SMAC G11 Grants Administration and Management workshop from 14th to 17th July 2025, aimed at strengthening grant management offices and systems among the participating universities and entities.
It is envisioned that through this capacity building approach, the workshop which brings onboard over 130 participants from different universities and entities, will address the knowledge and skills gaps among faculty, grant managers, administrators and support staff.
The participating universities and entities include: Makerere University, Uganda Christian University-Mukono, Soroti University, Gulu University, Clarke International University, King Ceasor University, Kyambogo University, Muni University, Mother Kevin University, Uganda Martyrs’ University-Nkozi, Ernest Cook University, Mbarara University of Science and Technology, University of Kisubi, Kabale University, Busitema University, BRAC University, Infectious Diseases Institute, Ministry of Health, and among others.
Makerere University and Northwestern University have built a strong partnership over the past decade through academic exchange, collaborative research, and capacity building initiatives. “Since 2020, the institutions have deepened their collaboration in research administration through the UASP fellowship, sharing best practices and co-developing of sustainable systems to strengthen research management,” said Prof. Sylvia Antonia Nakimera Nannyonga-Tamusuza, Head of Grants Administration and Management Support Unit (GAMSU) at Makerere University.
She informed the participants that Northwestern University has been instrumental in building the capacity of staff at Makerere University in grants writing, management and administration.

Prof. Nannyonga-Tamusuza testified that when she was appointed to head GAMSU, she received comprehensive training from Northwestern University, which enhanced her competences and expertise in the field. She acknowledged Kate Klein from Northwestern University for the mentorship that empowered her with valuable knowledge and skills. She reported that five (5) members of staff from Makerere University had been trained by Northwestern University in grants and research management.
Filled with joy, she introduced the team of experts from Northwestern University namely Kate Klein, Bethany Ekesa and Elizabeth Christian to Makerere University, and applauded them for accepting to be facilitators. Prof. Nannyonga-Tamusuza assured the workshop participants that the team from Northwestern University would not only train them, but would share best practices in grants management and administration as well as networking opportunities.
The training workshop is part of the Expanded Strengthening of Makerere University’s Research Administration Capacity (E-SMAC) program, which focuses on enhancing research administrative systems and staff capacity at Makerere University and its partner institutions. Mordecai Tayebwa is the Program Director and Principal Investigator of the E-SMAC program being implemented from July 2024 to December 2025. The program is funded by the National Institute of Allergy and Infectious Diseases (NIAID).
The workshop provides a platform to build faculty, grant managers and administrators capacity in grant writing and management, foster cross-functional collaboration across departments, strengthen understanding of budget creation, biosketch and funder systems, encourage mentorship and peer to peer learning, and lay a foundation for regular support.
The training tackles four broader themes namely Grants Introduction and Systems, Proposal Development, Capacity Building, and Outcomes and Forward Planning. It covers vital areas such as grant writing, budgeting, funder systems, compliance, and overall grant administration. It features practical sessions, mentorship opportunities, and collaborative learning, with the goal of strengthening pre-award and post-award grant management and improving research productivity and compliance.

Opening the workshop, the Acting Deputy Vice Chancellor (Finance and Administration) at Makerere University, Prof. Winston Tumps Ireeta urged universities to institutionalize grant management offices and policies as well as strengthening research systems through collaborations.
Sharing his experience, Prof. Ireeta informed the participants that he was involved in the strategic discussion that led to the establishment of GAMSU at Makerere University. “We observed that Makerere University School of Public Health had established a grants office, which was instrumental in attracting and winning funds for research. We were inspired by this best practice. Thus, a comprehensive policy was developed to streamline and strengthen grants management across all colleges at the University,” he said.
Prof. Ireeta noted that Makerere University commits to being a research-driven institution, a strategic direction, that needs a strong funding base. ‘Research grants are therefore a key resource,” he said.
Stressing the importance of adhering to the technical details in the grants management processes, Prof. Ireeta appealed to the participants to be active listeners and maximally utilize the moment to learn from the experienced facilitators.

In the same vein, Prof. Nannyonga-Tamusuza, applauded the University Council and Management for the strategic direction undertaken to elevate GAMSU from a Unit to a Directorate. This points to the central role of the grants office in the life cycle of Makerere University. She pointed out that GAMSU reports to the Vice Chancellor through the Deputy Vice Chancellor (Finance and Administration).
Established by the University Council in 2020, GAMSU is a central office at Makerere University. It provides professional and coordinated services across the entire grant life-cycle-from identifying funding and developing proposals to ensuring compliance, project execution, financial oversight, and institutional capacity building. GAMSU works closely with academic and administrative staff to support competitive, well-managed and accountable research.
Focusing on the training workshop, Prof. Nannyonga-Tamusuza called upon the participants to utilize the golden opportunity to deepen their understanding of grants management in advancing research. She acknowledged the role of this collaboration in fostering mutual learning and the sharing of best practices, noting that such initiatives were key in ensuring that research conducted by universities aligns with global standards. She encouraged participants to engage fully in the workshop, collaborate with their peers, and build lasting connections to foster continuous learning.
The Administrative Director of the Havey Institute for Global Health at Northwestern University, Kate Klein, noted that grants administration goes beyond securing funding. She explained that grant administration is about building strong, sustainable systems that support researchers, facilitate collaboration, and ultimately contribute to solving global challenges.
Klein stated that grants administration and management require continuous learning, adaptability, and a strong foundation in regulatory and financial oversight.
“Collaborating and learning from one another is essential,” Klein stated. “When grants administration is effectively managed, it becomes a powerful catalyst for driving impactful change in research, ultimately advancing global initiatives that address the world’s most pressing challenges.”

She urged participants to critically analyze their current systems and identify areas where improvements could be made. By doing so, they would be better positioned to manage grants effectively and maximize their impact. She guided that a research grants administrator should be able to design monitoring frameworks, liaising with funders to address grant-specific issues, coordinating compliance, budgeting and reporting to ensure timely and effective implementation.
Presenting the Existing Support Systems and Principal Investigator (PI) agreements, Prof. Nannyonga-Tamusuza pointed out the critical role of GAMSU in maximizing Makerere University’s access to grants. This is particularly important in the context of limited financial resources, where GAMSU ensures that the university effectively leverages available funding opportunities.
Prof. Nannyonga-Tamusuza explained that GAMSU ensures research projects align with the priorities of funders and comply with both institutional and external regulations. She emphasized that this alignment is essential for securing and managing grants successfully. She stated that oversight offered by GAMSU, helps streamline the process for researchers. She pointed out that grant management is a collaborative process, involving multiple stakeholders across the university, which ensures that the necessary expertise and support are in place to manage grants effectively.
Underscoring the importance of grant negotiations, particularly with sub-award grants, Prof. Nannyonga-Tamusuza clarified that such negotiations are most successful when managed at the institutional level, where GAMSU oversees the entire lifecycle of a grant-from identifying funding opportunities to post-award activities.
Harriet Nambooze, the Project Coordinator at Makerere University School of Health Sciences, provided participants with a detailed guide on navigating the National Institutes of Health (NIH) grant application process. She introduced essential tools such as Grants.gov, eRA Commons, SAM.gov and the NATO Commercial and Government Entity (NCAGE), which are critical for applying and receiving an NIH award.

Nambooze stressed the importance of accurately setting up roles in the eRA Commons system, including Signing Official (SO), Principal Investigator (PI), Account Administrator (AA), and Administrative Official (AO), as well as ensuring that profiles are up-to-date across various systems.
She highlighted the necessity of adhering to NIH’s strict submission deadlines and maintaining active individual and institutional profiles to facilitate timely applications. She recommended that institutions should appoint multiple Signing Officials (SOs), to avoid any delays with the required submissions.
Presenting to the participants, Mordecai Tayebwa shared a detailed, step-by-step guide to starting a new grant application. He explained the key elements of the grant process, including the necessity of including a budget, adhering to specific formatting guidelines, and uploading required documents, such as the foreign justification for international projects.

He pointed out the need of thoroughly verifying the application before submission to ascertain that all required documents are included. “This step is crucial to avoid errors that could delay or jeopardize the submission,” he said.
The first day of the workshop set a strong foundation for enhancing grant administration capacity among the participating universities. Participants were equipped with knowledge and skills in grant systems at the national and global levels.
Day two, will focus on topics such as reading funding opportunity announcements, tailoring writing, budget development and justification, sub-contract management, sub-recipient monitoring, and Memoranda of Understanding (MoUs).
On Day three, the participants will gain a deeper understanding of the Grants Office, financial management, internal controls and reporting, peer review process overview and project closeout.
On Day four, the participants will witness the launch of the MakGAP (Makerere University Grants Professional Initiative), listen to a keynote speech on grants management from the Vice Chancellor of Makerere University, Prof. Barnabas Nawangwe, as well as presentations on professional growth through MakGAP, CRA Exam, and Global Research Administration Networks, and professional recognition of research managers and administrators in Africa and post evaluation.
The first day of the workshop set a strong foundation for enhancing grant administration capacity among the participating universities. Participants were equipped with knowledge and skills in grant systems at the national and global levels.
Day two, will focus on topics such as reading funding opportunity announcements, tailoring writing, budget development and justification, sub-contract management, sub-recipient monitoring, and Memoranda of Understanding (MoUs).
On Day three, the participants will gain a deeper understanding of the Grants Office, financial management, internal controls and reporting, peer review process overview and project closeout.
On Day four, the participants will witness the launch of the MakGAP (Makerere University Grants Professional Initiative), listen to a keynote speech on grants management from the Vice Chancellor of Makerere University, Prof. Barnabas Nawangwe, as well as presentations on professional growth through MakGAP, CRA Exam, and Global Research Administration Networks, and professional recognition of research managers and administrators in Africa and post evaluation.
Health
Ugandan Study Flags Girls and Senior Students as a Mental Health High-Risk Group
Published
7 days agoon
July 12, 2025
Based on research led by Max Bobholz and colleagues from Makerere University in Uganda, Essentia Institute of Rural Health, and the Medical College of Wisconsin in the United States.
Adolescence is meant to be a time of holistic growth and self-discovery, but for many Ugandan teenagers, this period is becoming a season of silent mental health struggles. A new study published in PLOS Global Public Health has uncovered a silent but growing crisis: nearly one in five Ugandan secondary school students in the study areas have signs of an emotional disorder. These conditions included anxiety, depression, post-traumatic stress disorder (PTSD), and adjustment disorders often involving excessive worry, sadness, fear, or mood instability. Also, one in 20 adolescents exhibited behavioral issues ranging from attention-deficit/hyperactivity disorder (ADHD) and oppositional defiant disorder to substance use and other risky behaviors like alcohol use.
The study, led by Max Bobholz, a PhD candidate in Public and Community Health at the Medical College of Wisconsin, surveyed a sample of 1,953 students aged 10 to 18 years enrolled in eight secondary schools in Iganga district in Eastern Uganda and Mukono district in Central Uganda. This was one of the most comprehensive efforts yet to understand the prevalence and drivers of mental health challenges among school-going Ugandan adolescents.
“We are looking at a generation facing a complex blend of stressors, namely, academic, social, and emotional,” says Bobholz. “Our findings show that certain groups are especially vulnerable, and schools need to be equipped to respond.”
This study results, published on June 12, 2025 was funded by the Swedish International Development Cooperation Agency (SIDA), a government agency of the Swedish Ministry for Foreign Affairs, through the Makerere University Postdoctoral Fellowship to one of the investigators, Dr. Catherine Abbo. Other researchers included Julia Dickson-Gomez, Arthur Kiconco, Abdul R. Shour, Simon Kasasa, Laura D. Cassidy, and Ronald Anguzu.
According to the study, girls bear a higher emotional burden. Researchers found that female students had nearly two times higher odds of suffering from emotional disorders such as anxiety or depression than their male peers.
Dr. Catherine Abbo, an Adolescent Psychiatrist and Associate Professor at Makerere University, attributes this to both biological and socio-cultural factors. “Puberty brings hormonal shifts that can heighten emotional sensitivity,” she explains. “But just as importantly, Ugandan girls often face intense pressure to conform to gender roles while also navigating issues like body image, harassment, and future uncertainty.” The researchers are calling for gender-sensitive mental health interventions, particularly in schools, where early support could help mitigate long-term mental health issues.

Higher associations in older teens?
Age also emerged as a key associated factor, with each additional year increasing the odds of behavioral disorders by 20%. “As adolescents grow older, they are more prone to risk-taking, impulsivity, and resistance to authority,” explains Dr. Simon Kasasa, a senior lecturer and biostatistician at Makerere University School of Public Health.

“Combine that with academic pressure and identity-related stress, and it’s no surprise we’re seeing more conduct issues in late adolescence,” Dr. Ronald Anguzu, an Assistant Professor in the Institute for Health and Humanity at the Medical College of Wisconsin, added. This study raises critical questions about whether and how Ugandan secondary schools support older students as they transition toward adulthood.
The unseen influence of family mental health
The study also found that adolescents with a family history of mental illness had twice the odds of exhibiting behavioral problems compared to those without such a history.
“This speaks to the intersection of genetics and environment,” says Bobholz. “Living in a household with people affected by mental illness can mean instability, stigma, and lack of emotional support, all of which weigh heavily on a developing mind.”
The authors recommend that school mental health screening include family mental health history and advocate for greater collaboration between education and health sectors to support at-risk households.

Private schools: High marks, higher stress?
Interestingly, students in private schools had 1.4 times the odds of experiencing emotional disorders compared to those in public schools. Private schools, often seen as academic havens, may inadvertently be cultivating high-pressure environments. “There’s an assumption that better facilities mean better well-being,” says Dr. Abbo. “But intense academic competition, social isolation, and a lack of trained counselors can create emotional pressure cookers.”
Previous research in 47 secondary schools across five districts (Rakai, Kyotera, Masaka, Lwengo, and Kalungu) in southwestern Uganda found that economic and family support helped reduce absenteeism among adolescent girls in secondary schools. However, this support did not significantly improve behavior or reduce grade repetition. The region, which includes districts like Rakai and Masaka, also faces a higher burden of HIV, adding to the challenges young people experience.
Meanwhile, a review of data from 42 primary schools in Luwero District identified school-based mental health interventions such as cognitive behavioral therapy and mindset-building approaches as being particularly effective. Researchers now suggest that integrating these strategies, along with efforts to reduce school violence, could go a long way in improving the mental health of Ugandan adolescents.
A-Level pressure: Academic ambition meets mental health strain
The study also found a correlation between advanced (A’level) education and increased risk of emotional disorders. “We selected one school district from each region based on population and past academic performance. As these students prepare for university or the job market, the pressure to succeed becomes enormous,” says Kasasa. “They’re facing a future full of uncertainty, with very little structured mental health support to help them cope.”

A wake-up call for Uganda’s education and health systems
The authors of this study assert the urgent need for school-based mental health programs, especially in private and A-level institutions. These programs should offer routine screening, emotional support, and training for teachers to recognize warning signs of mental health disorders.
Importantly, this study adds weight to calls for a national adolescent mental health policy, tailored to Uganda’s context, with interventions that bridge health, education, and social services.
“Our data shows that mental health challenges are not a fringe issue,” says Bobholz. “They are widespread, significant, and deeply tied to school, home, and society.”
The COVID-19 school closures between 2020 and 2022 deepened feelings of isolation and financial strain, with out-of-school adolescents reporting depression rates as high as 21.5% to 50% higher than their peers who remained in class, according to research published in February 2025. Yet Uganda invests less than 1% of its health budget in mental health, with just one psychiatrist per million people, leaving many teens to cope through cheap alcohol used by 28% of urban youth or untrained healers, as reported by the government paper The New Vision in April 2025. With only 26% of students completing lower secondary school and 35% of the population under age 24, these mental health challenges now pose a serious threat to the country’s future.
Mercy Akankunda of Proven Foundation, a Ugandan NGO supporting vulnerable groups, warns that mental health struggles are quietly eroding the well-being of the country’s youth, over 12 million strong and making up 35% of the population. “These teens are not just statistics. They are the future of Uganda, she asserts. If Uganda hopes to reap the dividends of its young population, addressing adolescent mental health must become and remain a national priority, not just for treatment, but for prevention, resilience, and hope.
Reference:
Bobholz, M., Dickson-Gomez, J., Abbo, C., Kiconco, A., Shour, A.R., Kasasa, S., Cassidy, L.D., & Anguzu, R. (2025). Correlates of behavioral and emotional disorders among school-going adolescents in Uganda. PLOS Global Public Health. Read the study here
Health
Call for Applications: Responsible Conduct of Research (RCR) Training Course
Published
1 week agoon
July 11, 2025By
Mak Editor
The Responsible Conduct of Research (RCR) Training Course, scheduled to take place from July 30th to August 1st, 2025, at the Makerere University College of Health Sciences’ Conference Room.
Background
The SUSTAIN: Advancing Makerere University Masters of Health Sciences in Bioethics program at Makerere University College of Health Sciences aims at developing and institutionalizing a mentorship program in research ethics that facilitates development of bioethics professionals and health researchers who are committed to the growth and application of research ethics in Uganda’s academic and research institutions to the highest possible degree. The Responsible Conduct of Research (RCR) course is one of the short courses that introduces trainees to a framework that involves application of established scientific, professional norms and ethical principles in the performance of all activities related to scientific research.
Course objectives
At the end of this course, trainees should be able to identify, manage and prevent research misconduct.
Course outline
Introduction to RCR; Introduction to Professionalism and Ethics; Human subject’s protection and regulatory framework in Uganda; Humane handling of animal research subjects; Conflict of interest;
Responsible laboratory practices; Mentor-mentee relationships; Collaborative research international, industry); Peer review; Research misconduct (including policies for handling misconduct); Community involvement during research in a low resource setting; Responsibility to society and environment; Responsible financial management; Data acquisition, management, sharing and ownership; Responsible authorship, publication and communication.
Target group
The Responsible Conduct of Research course is targeted at Researchers, Research administrators, Research assistants, Study coordinators, Graduate students and Student supervisors. Certificates will only be awarded to participants with 80% attendance.
Course fee: 205,000/=, or 56USD is payable.
The course fee will cater for meals and refreshments during the training period.
Payment & Registration procedure:
9030026194023, Stanbic Bank, Mulago, Makerere University Biomedical Research Center Limited
Dollar Currency:
9030026194147, Stanbic Bank, Mulago, Makerere University Biomedical Research Center Limited
Please Note: Share payment details on email/whatsup and a hardcopy deposit slip delivered on the first day of the training to Miriam Musazi, Department of anatomy, Bioethics Centre, Room C4,
Mob: +256 782 363 996/ +256 701 363 996, Email: mmusazi@gmail.com.
NB. Only those who will have paid by this date will be considered for the course
Venue: The training will take place at Makerere University College of Health Sciences’ Conference room
Trending
-

 General2 weeks ago
General2 weeks agoRe-advert: Admission to Undergraduate Programmes 2025/2026
-

 General1 week ago
General1 week agoRe-Advert for Applications for Diploma and Certificate Training
-

 General5 days ago
General5 days agoMakerere University Fees Waiver for 40 First Year Female Students 2025/2026
-

 General2 weeks ago
General2 weeks agoPress Statement on Ranking
-

 Health1 week ago
Health1 week agoCall for Applications: Responsible Conduct of Research (RCR) Training Course
