Health
Researchers Recommend Drug to Win the Malaria War in Children
Published
5 years agoon

“Malaria is a terrible disease. It affects you beyond discharge. Once treated for malaria, you are susceptible to more infections, and the chances for re-admission are very high.”
Uganda’s fight against malaria has received a boost after medical researchers recommended that a wonder drug that has produced positive results in Uganda, Kenya and Malawi be embraced globally.
Results of the study showed that treatment with Dihydroartemisinin–Piperaquine (DP) should now be the preferred treatment for malaria in both children and adults after discharge. The trials in children indicated reduced number of deaths from severe malaria by 80 per cent.
The study-the Malaria Chemoprevention in the Postdischarge management of severe Anemia was carried out over a two-year period at Jinja, Kamuli, Hoima, Masaka and Mubende Regional Referral hospitals and studied 1,049 children with severe malaria, which kills nearly a million people each year, mainly young children and pregnant women.

“We focused on those hospitals because those are the areas that are most hit with Malaria.We found out that Children who have been hospitalized with severe anemia in areas of Africa in which Malaria is endemic have a high risk of readmission and death within 6 months after discharge,” said Dr. Robert Opoka, a Senior Lecturer at the Department of Paediatrics and Children Health, Makerere University College of Health Science.
Dr. Opoka noted that they allocated children with severe malaria with antimalarial during the first 3months post-discharge at 2,6 and 10 weeks and they were followed for three months and found out that 80 percent of the children on the antimalarial survived.
“It was observed that there was 70% significant reduction in either deaths or re-admissions among the children receiving the antimalarials compared to the group of children who were not on admission,” Dr. Opoka noted.

The study, whose findings have been published in the latest edition of the New England Journal of Medicine (NEJM), was funded by the Norwegian Research Council. It involved an international consortium of researchers. Some of the members of the research team from Makerere University College of Health Sciences included: Dr. Richard Idro, Dr. Aggrey Dhabangi and Dr. Robert Opoka
Malaria is caused by parasites that are injected into the bloodstream by infected mosquitoes. Severe malaria is often the main reason why children are admitted to hospital in sub-Saharan Africa, and one in 10 of these children die.
The Ministry of Health 25th Health Sector Joint Review report 2018/2019 showed that malaria was still the leading cause of admissions for all ages accounting for 32.9 per cent of all admissions.

“The drug has a huge impact on reducing mortality and morbidity in children under five-years recovering from severe malaria. The children who were not on antimalarials developed respiratory distress, complicated seizures, movement disorders, vision impairment, speech and language impairments, cognitive deficits, epilepsy and destructive behavior,” said Dr. Aggrey Dhabangi, a Lecturer at the Makerere University College of Health Sciences.
Dr. Dhabangi noted that DP is available in both private and public pharmacies. And a dose goes for UGX 3,000 for children and UGX 3,500 for adults and it is supposed to be taken for 3days in a month. “(DP) is a reliably oral effective drug, and it is given to children according to weight and it should be given 14days after discharge and later after a month,” Dhabangi noted.
During the meeting held on 3rd December 2020, Dr. Richard Idro, a Senior Lecturer at the Makerere University College of Health Sciences, revealed that further studies in Malawi have demonstrated that delivery of the drugs using community-based approaches is associated with much higher adherence 24% than hospital-based approaches.

“These children are readmitted or die because by the time they are discharged from the hospital they have not fully recovered so when they go back home especially to places with high infections, they get attacked again, but with the antimalarial they get protected until they recover and gain their immunity,” Dr. Idro noted. The researchers recommended that after discharge, the children should be given Multi-Vitamin supplementation and use mosquito nets.
Responding to the findings, Dr. Charles Olaro, the Director of Curative Services at the Ministry of Health, said that he was happy with the research findings and promised to translate the research findings into policy so that Children in Uganda are saved.

“Malaria is still one of the diseases burdening clinical services, so we still need more research and innovations in that area. We need to start up a package where health workers do not only stop at discharging patients but also educate them about the post discharge,” Dr. Olaro, noted. He assured the public that the Ministry of Health had stocked enough Dihydroartemisinin-Piperaquine (DP) for public hospitals.
The Vice Chancellor of Makerere University, Prof. Barnabas Nawangwe who was represented by Dr. Sabrina Kitaka from the College of Health Sciences commended the research team comprising Makerere University researchers for creating a paradigm shift that focuses on only treatment of malaria to a preventive approach that will save lives. The Vice Chancellor expressed Makerere University’s readiness to review the curricula to include prevention of malaria and chemo prevention in the management of malaria. Noting that the researchers focused on three (3) months after discharge, he appealed to research team to consider an option of extending the period of follow up to six (6) months so that more lives are saved.

Dr. Jimmy Opigo, the Assistant Commissioner-Health Services at the National Malaria Control Division said: “We are happy that this PMC study has enabled people to realise that treatment of malaria and discharge is not enough. There is need for longitudinal management of those discharged. The medical team and health care workers should add patient education and improve health care practices in the management of malaria.”
Article by Mak Public Relations Office
You may like
-


Mak Selected to Host Alliance for African Partnership Africa Office
-

Climate variability found to shape malaria trends in Yumbe District
-


Mak hosts First African Symposium on Natural Capital Accounting and Climate-Sensitive Macroeconomic Modelling
-


Makerere Launches Scholarly Guide, Calls for Increased Research, Publication and Innovation in Africa
-


When Birth Becomes the Most Dangerous Moment, Wanduru & the Work of Making Labour Safer
-


How Jimmy Osuret Turned Childhood Trauma into Evidence for Safer School Crossings
Health
MakSPH Environmental Health Graduates Trained to Prevent Disease at Its Source
Published
1 day agoon
February 24, 2026
In most health systems, attention turns to illness after it appears in clinics and hospitals. Environmental Health works earlier, often invisibly, by preventing disease before treatment becomes necessary. At Makerere University School of Public Health (MakSPH), this preventive philosophy shapes the training of students learning to manage health risks at their source, through sanitation systems, safer environments, community engagement, and evidence-based public health action.
This year, as MakSPH presents 29 graduands approved by the Makerere University Senate for the award of the Bachelor of Environmental Health Science (BEHS) degree, four outstanding students graduate with first-class honours. Their journeys, shaped by different personal histories and professional ambitions, provide a clear view of how the School prepares practitioners whose work begins long before patients reach health facilities. Through academic training, field practice, research exposure, and leadership experience, the programme equips graduates to address the environmental and social conditions that determine health outcomes across communities.

Environmental health occupies a distinctive position within public health practice. Rather than focusing primarily on diagnosis or treatment, practitioners work at the intersection of science, policy, and society, addressing risks linked to water and sanitation, food safety, occupational health, climate change, and urbanisation. The discipline demands technical competence alongside communication, systems thinking, and community engagement, capabilities that increasingly define modern public health leadership.
The journeys of Nakulima Bushirah, graduating with a CGPA of 4.58 on February 25, 2026, Mujurani Alphersiiru with 4.44, and Cherop Eric with 4.41, alongside Phillip Acaye, the cohort’s overall best student with a CGPA of 4.63, demonstrate how MakSPH shapes students from varied beginnings into professionals grounded in prevention. Their paths reveal a shared formation that links classroom learning with real-world health challenges and prepares graduates to prevent disease before it occurs.
Bushirah Nakulima’s Turn Toward Prevention

For Bushirah Nakulima, environmental health began during a period of uncertainty. The COVID-19 pandemic repeatedly disrupted her Bachelor of Pharmacy studies at Kampala International University, prompting reflection about the kind of health professional she wanted to become. A conversation with a family friend working in preventive health introduced an alternative path, one focused not on treating illness after onset but on preventing it altogether.
“When I applied to Makerere University in 2022, I was considering two career paths,” she recalled. “I prayed to Allah to guide me toward the best one. When I was admitted to the Bachelor of Environmental Health Science, I accepted it wholeheartedly, and I came to appreciate it even more as I studied.”
Her academic foundation had already demonstrated consistency. She progressed from Melody Junior School in Nansana, where she obtained aggregate eight in 2010, to Shuhada’e Islamic School in Nyamitanga, completing O-Level with 25 aggregates in 2016 and A-Level with 10 points in 2018. Pharmacy initially appeared the logical continuation, yet environmental health offered something broader in scale and impact.
“Environmental Health offered an opportunity to prevent illness and suffering before it occurs,” she explained. “It allows a single intervention, such as WASH or health education, to protect many people at once, and it provides flexibility to work across diverse environments. It offered freedom to operate in various settings, which truly connects with my personality since I love exploration.”
At MakSPH, classroom concepts quickly translated into practice. During her internship at Mukono Municipal Council, she conducted school health education sessions, participated in inspections of markets and abattoirs, and engaged communities facing sanitation challenges. Field exposure deepened her understanding of how environmental conditions directly shape disease patterns, reinforcing prevention as both a scientific and social responsibility.
Leadership further expanded her training. Serving as the 90th Female Guild Representative Councillor (GRC), she represented the School of Public Health in the Student Guild structure, facilitating engagement between students and School leadership on academic and welfare matters. The role strengthened her capacity for representation, negotiation, and collaborative problem-solving, skills central to public health practice, where advocacy and systems engagement are inseparable from technical expertise.
Graduating with a CGPA of 4.58, Bushirah’s research examined roadside vendors’ exposure to air pollution in Kampala, reflecting growing concern about occupational and urban environmental risks. She now plans to pursue advanced training in public health, building on MakSPH’s emphasis on evidence-driven and community-centred practice.
Cherop Eric’s Return to the Classroom

Eric Cherop’s journey into environmental health began not in lecture halls but in community service. Raised in Kapchorwa District, he was shaped by economic hardship and resilience, experiences that informed his commitment to community well-being.
He completed his Primary Leaving Examinations at Chema Primary School, a Universal Primary Education institution, attaining 24 aggregates in 2008. He later joined Sipi Secondary School, where he obtained 37 aggregates at Uganda Certificate of Education in 2012 and continued at the same school for A-Level, earning 8 points at Uganda Advanced Certificate of Education in 2014.
After earning a Diploma in environmental health sciences from Mbale School of Hygiene between 2015 and 2017, he entered public service as an Environmental Health Officer and Community Field Facilitator with Kapchorwa District Local Government. His work included sanitation campaigns, climate resilience initiatives, nutrition education, and household behaviour change programmes. Over time, field experience revealed the limits of practice without deeper theoretical grounding.
“I wanted to understand not only what works in communities, but why it works,” he explains. Enrolling in the BEHS programme at MakSPH in 2022 allowed him to connect practical experience with analytical training. Coursework strengthened competencies in environmental risk assessment, participatory engagement, and data-driven planning. Mentorship reshaped how he interpreted evidence.
“My lecturers helped me move beyond seeing data as numbers,” he said. “I learned to see it as evidence that guides decisions and improves accountability.” Graduating with a CGPA of 4.41, Eric now aims to advance evidence-driven leadership at the intersection of climate change, nutrition, and environmental health, ensuring interventions remain grounded in community realities.
Mujurani Alphersiiru’s Path into Environmental Health

For Mujurani Alphersiiru, Environmental Health arrived at an unexpected moment, when his academic future appeared uncertain. Financial pressures had begun to threaten the continuation of his Bachelor of Nursing Science studies at Kampala International University Western Campus, raising the real possibility that his university education might end prematurely. The turning point came when the government district quota admission list was released, offering him placement at Makerere University under Bunyangabu District and opening an alternative academic pathway he had not previously considered.
At the time, environmental health was unfamiliar to him. “I didn’t know what environmental health was,” he recalls. “But I celebrated because I had reached my dream university.” Orientation sessions and early coursework gradually reframed that uncertainty, revealing a discipline grounded in prevention, systems thinking, and public health policy. What began as an unexpected opportunity soon developed into a clear professional direction.
Serving as class president and 90th Male GRC for the School with Nakulima Bushirah, Mujurani organised student activities, mobilised community outreach initiatives, and advocated for improved learning environments. Balancing leadership responsibilities with academic performance required deliberate discipline and time management.
His educational foundation began at St. Augustine Butiiti Demonstration Primary School in Kyenjojo, where he scored 12 aggregates in 2014. He later attended Pride Secondary School in Mityana, attaining 25 aggregates at O-Level in 2018, before proceeding to Kibiito Secondary School in Bunyangabu, where he obtained 13 points at A-Level in 2021, performance that earned him government sponsorship for university education. At MakSPH, faculty mentorship further strengthened both his academic rigour and commitment to public service.
“Government sponsorship meant responsibility,” Mujurani said. “I had to plan my time carefully while remaining active in school programmes.” Graduating with a CGPA of 4.44, his interests now centre on governance and accountability within health systems, particularly strengthening the implementation of public health policies.
Training Prevention Professionals
Taken together, the three journeys demonstrate how MakSPH’s Environmental Health training converts diverse personal backgrounds into a shared professional orientation centred on prevention. Through interdisciplinary coursework, field placements, research mentorship, and leadership opportunities, students develop competencies that extend beyond technical knowledge to include systems thinking and public engagement.

The BEHS programme, established in 2000 within MakSPH’s Department of Disease Control and Environmental Health, remains the School’s only undergraduate degree and has trained more than 1,000 graduates who now serve across government institutions, non-governmental organisations, academia, and international health programmes. Its continued evolution reflects growing recognition that strengthening health systems requires professionals capable of addressing environmental risks before illness occurs.
The achievements of this year’s graduates, therefore, represent more than academic distinction. They reflect a model of training designed to prepare professionals whose work reduces the need for treatment by preventing disease at its source, reinforcing MakSPH’s role in shaping Uganda’s environmental health workforce.
Health
Makerere University School of Public Health Graduates First Cohort of Cost-Effectiveness Analysis Short Course
Published
5 days agoon
February 20, 2026By
Mak Editor
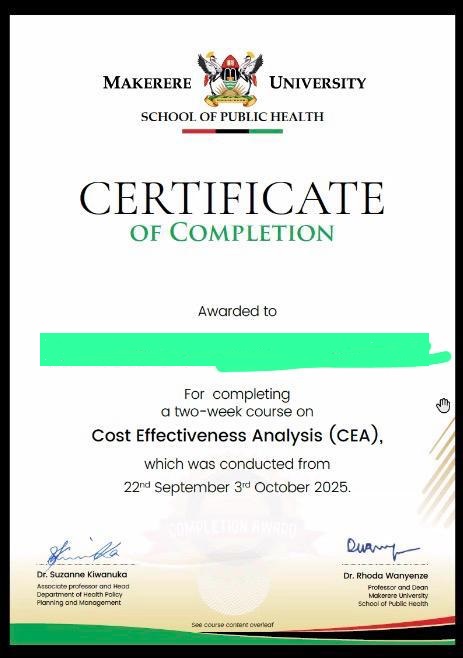
Kampala, Uganda – The Makerere University School of Public Health (MakSPH) has marked a significant milestone with the graduation of the first-ever cohort of its Cost-Effectiveness Analysis (CEA) Short Course. The pioneering programme is designed to strengthen capacity in economic evaluation in Uganda and beyond.
The virtual graduation ceremony honored eleven (11) participants who completed the course. The cohort included professionals from academia, research institutions, government agencies, and non-state actors, reflecting the increasing demand for skills in economic evaluation across sectors.
The short course was developed and implemented by the Department of Health Policy, Planning, and Management (HPPM) in response to the increasing need for evidence-informed decision-making in a context of limited resources.
In her remarks during the ceremony, Assoc. Prof. Suzanne Kiwanuka, Head of the Department of Health Policy, Planning and Management (HPPM) at MakSPH, congratulated the inaugural cohort for completing what she described as a “critical and timely” course.
“With decreasing resources and rising demand for services driven by population growth and the emergence of high-cost technologies, decision-makers must make difficult choices,” she noted. “Cost-effectiveness analysis is no longer optional. It is central to conversations in the corridors of power.”
The CEA short course was designed to equip policymakers, researchers, and practitioners with both theoretical knowledge and practical skills in economic evaluation. Participants were introduced to key principles of health economics, costing methodologies, decision-analytic modelling, Markov modelling, sensitivity analysis, and interpretation of incremental cost-effectiveness ratios (ICERs).
According to Prof. Elizabeth Ekirapa, the course lead at MakSPH, this inaugural offering had been “a long time coming,” following years of discussions within the department about building local expertise in economic evaluation.
Delivered over 10 days through interactive online sessions, the course combined lectures, case studies, and hands-on modelling exercises using contextually relevant datasets. Participants were required to develop and present applied cost-effectiveness projects as part of their assessment, allowing them to translate theory into practice.
During the feedback session at the graduation ceremony, faculty emphasized the importance of clarity in defining study perspectives, selecting appropriate outcomes, and aligning research questions with modelling approaches.
Dr. Chrispus Mayora, one of the facilitators, highlighted the need to carefully select outcomes that directly reflect the intervention being evaluated. “When thinking about outcomes, ask yourself: Is this aligned with what I want to study? Interesting outcomes are not always the most appropriate ones,” he advised.
Participants were also encouraged to select modelling techniques such as decision trees or Markov models based on the research question and the nature of the disease or intervention under study.
Prof. Ekirapa described the graduates as “trailblazers,” noting that their feedback would shape future iterations of the course. “When you are the first cohort, you are like pioneers,” she remarked. “We are committed to improving this course to ensure it becomes a world-class programme.”
For many attendees, the graduation ceremony was a new experience, as certificates were awarded virtually an approach that participants welcomed as innovative and inclusive.
“Cost-effectiveness analysis enables us to maximise value for money,” noted Dr. Crispus Mayora of MakSPH. “It allows decision-makers to compare interventions systematically and ensure that limited resources achieve the greatest possible benefit.”
The programme aligns with Makerere University’s broader mandate to provide high-quality training that responds to national and regional development priorities. Participants who successfully complete the course receive a certificate signed by the Dean of the School of Public Health.
As the ceremony concluded, faculty encouraged continued engagement beyond the classroom. Graduates were urged to refine their project ideas and collaborate with the department in advancing research and policy discussions.
The successful completion of the first CEA short course marks an important step in building a cadre of professionals equipped to conduct rigorous economic evaluations. With plans to expand and refine the programme based on participant feedback, the HPPM department under MakSPH is positioning itself as a regional leader in health economics and policy analysis training.
Health
Uganda has until 2030 to end Open Defecation as Ntaro’s PhD Examines Kabale’s Progress
Published
7 days agoon
February 18, 2026
Silhouettes slip along narrow paths, farmers heading to their gardens, women balancing yellow jerrycans on their hips, children in oversized sweaters hurrying to school, and herders steering cattle toward open pasture, each movement part of a choreography older than memory. This is a quiet ritual in Kabale’s terraced hills, moments before the sun lifts.
The quiet procession to ahakashaka, or omukishaka, often sees figures moving quickly along familiar footpaths in the half-light, as children and adults walk with the urgency of habit. It is not a stroll but often a small, hurried run before daylight exposes what should be private.
It is February 2026, and the century-old Makerere University is celebrating its 76th Graduation Ceremony. The world paces and races toward artificial intelligence and digital revolutions. But some families still begin their day by rushing to the bushes for relief and concealment, while others engaged in economic activities such as gardening and grazing have no sanitation option other than using their surroundings to respond to the nature call!
The deadline to end open defecation is 2030. The science is settled, and the commitments are written into Sustainable Development Goal 6. Yet in parts of Kabale, only a small fraction of households is truly open defecation free.
In his PhD research, Dr. Moses Ntaro did not start with global targets or conference declarations. He began where the morning run ends, at the edge of the compounds, behind banana stems, along worn paths leading to Omukishaka. He asked whether students, equipped not with bricks but with conversation, follow-up, and persistence, could help communities replace that dash with something quieter: a door that closes.
What he found is both hopeful and unsettling. Change is possible. But dignity, like sunrise, should not require a run. And with 2030 approaching, time is no longer generous.

The Question That Would Not Let Him Go
Ntaro did not encounter open defecation as a statistic. While on foot and serving as Assistant Coordinator of Community-Based Education at Mbarara University of Science and Technology (MUST), he learned while supervising students placed in rural communities across southwestern Uganda. They walked villages together, conducted transect walks… and they observed.
“In my role as academic coordinator,” he explains, “students always took me on transect walks within the villages to show me how high open defecation practice was. The effect was evident in the high prevalence of intestinal infections we saw in health facility records.”
The link between sanitation and disease was not theoretical but visible in clinic registers. Diarrhea, intestinal worms, recurring infections among children, and more were all visible in the clinic registers.
Nineteen years ago, in 2007, Uganda adopted Community-Led Total Sanitation (CLTS), a strategy designed to trigger collective behavior change and eliminate open defecation. Progress, however, remained uneven. That same year, Ntaro was working as an Environmental Health Officer with the Water and Sanitation Development Facility under the Ministry of Water and Environment. He was three years away from completing his Environmental Health degree at Makerere University School of Public Health.
And so, the question emerged, to Ntaro, that, ‘If students are already embedded in these communities through COBERS placements, why are we not intentionally harnessing them to accelerate sanitation change?’
That question became his PhD.

This is a Crisis That Should No Longer Exist
Globally, more than 350 million people still practice open defecation. Sub-Saharan Africa carries a disproportionate share. SDG 6, specifically Target 6.2, commits the world to ending open defecation and ensuring universal access to safe sanitation and hygiene by 2030. It prioritizes women, girls, and vulnerable populations. It speaks of dignity, of safely managed services, and of disease prevention.
We are four years away from that deadline. And in rural Kabale District, somewhere in southwestern Uganda, Ntaro’s research found that only 3 percent of households were truly open defecation-free.
Yes, three percent. His 2025 BMC Public Health study examined 492 residents. The average age was 49. Nearly 30 percent had no formal education. Most were women, the custodians of household hygiene and child health.
The determinants of Open Defecation Free (ODF) status were deeply behavioral.
Male-headed households had higher odds of being ODF. Households with clean compounds, clean latrine holes, and consistent handwashing practices were significantly more likely to sustain sanitation improvements.
Sanitation, Ntaro realized, is not only infrastructure but also power, memory, habit, and social expectation.
“Factors associated with ODF status were not just economic,” he notes. “They were behavioral and contextual.”

Why It Feels So Wrong to Still Discuss This
Talking about open defecation in 2026 feels unsettling for three reasons. First, it feels like a failure of basic dignity.
Think of an era of global connectivity and rapid technological advancement, and hundreds of millions still lack privacy. For women and girls, this exposes them to harassment, exploitation, and fear. Sanitation is not just about disease but safety.
Second, it feels like an avoidable health crisis. One gram of feces can contain millions of viruses, bacteria, and parasites. Open defecation directly fuels cholera, typhoid, diarrhea, and environmental enteropathy, a silent contributor to child malnutrition and stunting. The science is settled, and yet the practice persists.
Third, it feels like a poverty trap. Illness leads to lost productivity; lost productivity deepens poverty, and poverty limits investment in sanitation. The cycle continues.
“Open defecation is not simply a sanitation issue,” Ntaro says. “It is linked to poverty, nutrition, and broader development.”

Testing a Different Approach
Ntaro’s doctoral thesis, “Effect of Student Community Engagement on Open Defecation-Free Status,” tested whether health profession students could effectively facilitate Community-Led Total Sanitation.
In some villages, traditional Health Extension Workers led the sanitation process. In others, trained students facilitated it under the COBERS (Community-Based Education, Research, and Service) model, which places medical trainees in community health facilities to learn through real-world practice, bridging classroom theory with primary care and public health work in rural settings.
Through this model, students led triggering, follow-ups, and community engagement. Open defecation declined. More households achieved Open Defecation Free status. And the cost per household was lower than in traditional approaches.
“Students were more effective,” Ntaro explains. “More households became open defecation-free compared to the traditional approach. And they were a cheaper human resource.”
But cost was not the real breakthrough. Presence was. Students stayed for weeks. They returned to check on latrines. They built trust. They kept coming back. Because sustainability, Ntaro argues, is not built in a single visit. It is built in repetition.
“There is a need for continued follow-ups and continued student engagement if long-term impact is to be realized.”
Change cannot be declared once and forgotten.

Behavior… and Not Just Bricks
Using the RANAS framework, Ntaro found that households that remembered to wash hands and kept latrines clean were far more likely to sustain Open Defecation Free status. In sanitation, behavior leaves evidence.
“Behavioral change interventions that empower communities,” he recommends, “such as CLTSH, should be strengthened to increase households with ODF status.”
In other words, building latrines is not enough, but communities must believe in them.

The Defense and the Countdown
On December 11, 2025, Ntaro defended his PhD. Examiners pressed him on scale and sustainability. Could student engagement be institutionalized? Could universities be embedded in district sanitation planning?
His answer was pragmatic: “Yes, but community-based education must be included in planning and budgeting.”
Four years remain to meet SDG 6.2. Four years to end open defecation and turn dignity from promise into practice. In 2026, this conversation should feel outdated. Instead, it remains urgent.

The Slow Work of Restoration
In Kabale, progress does not look dramatic. It looks like a latrine door closing firmly behind someone, a handwashing station with water and soap, a compound swept clean. It looks like a child who does not fall ill this month. Public health victories are often quiet.
As Makerere University approaches its 76th Graduation Ceremony, Dr. Ntaro Moses stands among its PhD graduands not with theory alone, but with evidence that change can be accelerated by reimagining who leads it. Students, he shows, are not only learners. They are the workforce, facilitators, and bridges between policy and path.
The hills of Kabale still wake under mist. But in more compounds now, privacy exists where bushes once stood open. Dignity is not restored in headlines, but one household at a time.
And with 2030 approaching, Ntaro’s work leaves a final, unavoidable question: if we already know how to end open defecation, if we already have the tools, the evidence, and the people, what, exactly, are we waiting for?

— Makerere University School of Public Health Communications Office, Graduation Profiles Series, 76th Graduation Ceremony
Trending
-

 Humanities & Social Sciences2 days ago
Humanities & Social Sciences2 days agoMeet Najjuka Whitney, The Girl Who Missed Law and Found Her Voice
-

 Health7 days ago
Health7 days agoUganda has until 2030 to end Open Defecation as Ntaro’s PhD Examines Kabale’s Progress
-

 Agriculture & Environment5 days ago
Agriculture & Environment5 days agoUganda Martyrs Namugongo Students Turn Organic Waste into Soap in an Innovative School Project on Sustainable Waste Management
-

 General7 days ago
General7 days agoMastercard Foundation Scholars embrace and honour their rich cultural diversity
-

 Health2 weeks ago
Health2 weeks agoCall for Applications: Short Course in Molecular Diagnostics March 2026
