Health
Prof. Serwadda Urges Shift from Transactional to Equitable Research Partnerships
Published
4 months agoon

On August 20, 2025, Makerere University School of Public Health (MakSPH) convened a timely workshop on Strengthening Equitable Partnerships in International Research Collaboration in Uganda. Held at the MakSPH Auditorium, the event brought together researchers, policymakers, and institutional leaders to reflect on how Uganda, and indeed the wider region, can engage more effectively and derive greater benefit from global research collaborations.
Delivering the keynote address, Prof. David Musoke Serwadda, a Professor Emeritus at Makerere University and a globally recognised HIV researcher and epidemiologist, urged a rethinking of how international research partnerships are structured. A former head of the Institute of Public Health (IPH) and later Dean of the School, serving between 2003 and 2009, Serwadda is also the founding director of the Rakai Health Sciences Programme (RHSP), which is one of Uganda’s most influential research initiatives on HIV. While acknowledging the many benefits Uganda has gained from global research collaborations, he cautioned that too many times, these partnerships remain transactional, shaped by donor priorities, bound to project cycles, and offering limited long-term value to local institutions once projects close.
Prof. Serwadda, himself a globally recognised and well-accomplished researcher, with over four decades of experience and numerous awards for his contributions to science and global health, observed that Ugandan partners are many times included in research projects for visibility rather than substance, often excluded from core roles such as Principal Investigators or from influencing agenda-setting, budget control, and authorship. “Partnerships are not an end in themselves; they exist to help us achieve mutually agreed objectives built on shared responsibility and reciprocal obligations. Too often, Southern institutions are brought into projects late, simply for optics. That is not equitable collaboration,” he insisted.
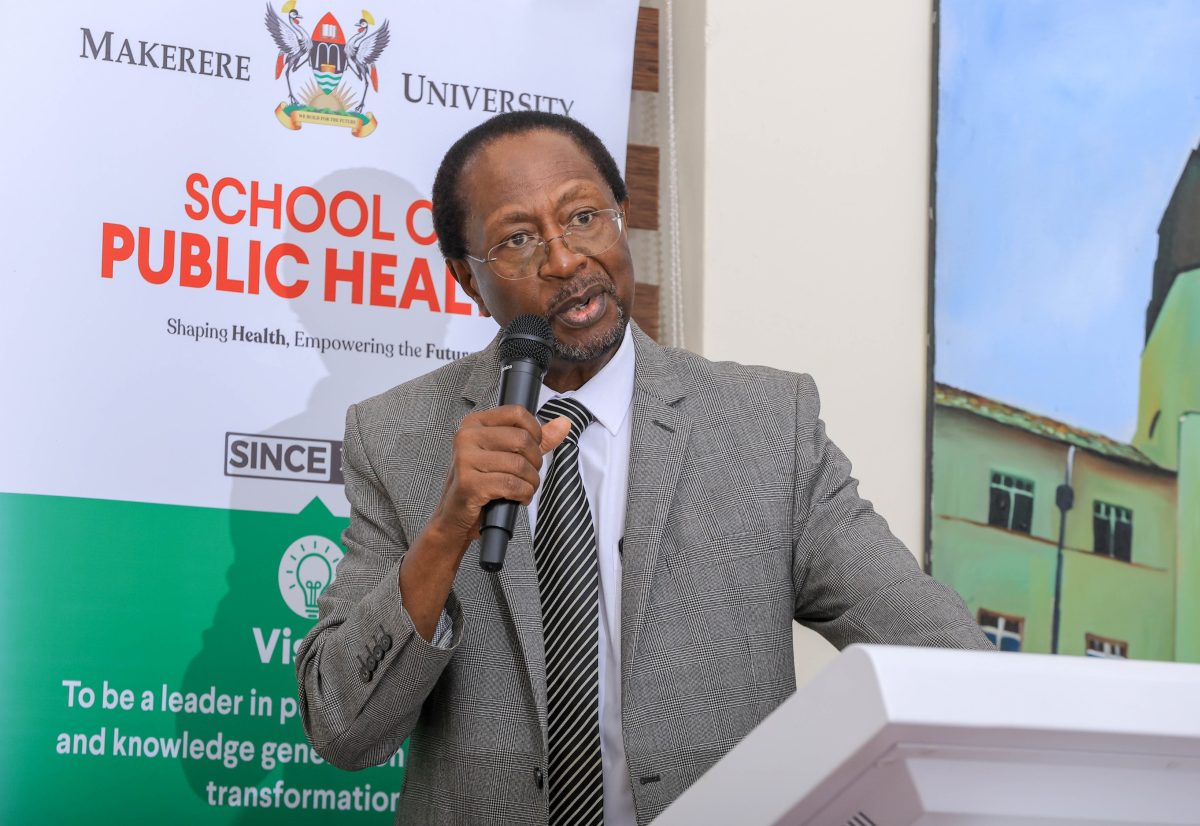
During his talk, he stressed that this imbalance undermines both research quality and sustainability, noting that normally, when local researchers are sidelined, studies often fail to align with national priorities or build capacity that endures. By contrast, partnerships that are grounded in mutual respect, fair resource sharing, co-design, and shared decision-making have the impact of producing knowledge that is globally relevant and locally impactful.
“Equity in partnerships is about fairness, ensuring that all partners, regardless of context, can contribute meaningfully. This also requires responsibility on our part in the Global South. We must insist on involvement from project conception, negotiate fair terms, and strengthen our own systems to manage collaborations effectively,” Prof. Serwadda advised, emphasising that strong institutions, clear strategy, agenda and objectives are key for local institutions to engage in mutually fair and beneficial research collaborations at the global and continental stage.
As Director and later Dean of MakSPH, Prof. David Serwadda spearheaded numerous research collaborations and attracted substantial grants that elevated the School and the University’s global standing. Today, MakSPH is recognised as Makerere University’s flagship unit for its wide-ranging partnerships and robust research management systems. Since its beginnings as a small Department of Preventive Medicine in 1954, through its transformation into the first Institute of Public Health in sub-Saharan Africa in 1975, its elevation to School status in 2007, and most recently its reinstatement as a standalone School with college status within Makerere University in January 2025, a status first granted in 2001, MakSPH has built a 70-year legacy of advancing public health through research, training, and policy engagement.
The School’s evolution, as often couched by its leadership, has been anchored on strategic and strong partnerships. These collaborations, be they local, regional or global, have driven health systems innovation, strengthened capacity, and informed policy, making partnerships the cornerstone of the School’s past achievements and future ambitions. At the celebration of the School’s 70th Anniversary, marked in December 2024, Makerere University Vice Chancellor Prof. Barnabas Nawangwe hailed MakSPH’s research output, community impact, and strong partnerships cultivated throughout the years. The Mak VC cited the School’s pioneering role in the HIV response led by Prof. Serwadda in the 1980s, the establishment of nutrition centres such as the Mwana Mugimu Unit at Mulago Hospital and across Uganda by the late Prof. John Kakitahi in the 1990s with support from Rotary International, and community projects like Kasangati Health Centre along Gayaza Road with support from the Rockefeller Foundation in the late 1950s, which advanced public education on healthy environments and wellness.

“The School of Public Health brings in almost half of all research grants at Makerere University, both in number and value, and these partnerships have been central to tackling Uganda’s public health challenges. From pioneering HIV/AIDS work that shaped global prevention strategies to interventions in maternal health, malaria, and infectious diseases, MakSPH has consistently combined academic excellence with community service. Its leadership during the COVID-19 pandemic further showed its ability to respond to national health emergencies with evidence-based solutions that directly benefit the people,” Prof. Nawangwe said with gratitude for the work done by the School through collaboration.

In 2024, the School had over 350 peer-reviewed publications in high-impact international journals as a result of this wide network and partnerships. MakSPH currently maintains a strong mix of North–South and South–South collaborations. Within the continent, the School is actively working in more than 25 countries, often partnering with multiple institutions within individual countries to advance research, capacity building, and policy influence. One such recent collaboration is the Partnership to Enhance Technical Support for Analytical Capacity and Data Use in Eastern & Southern Africa (PERSuADE) Project, funded by the Global Fund. Under PERSuADE, MakSPH, the prime grant recipient, hosted the secretariat led by Dean Prof. Rhoda Wanyenze as Principal Investigator, tasked with overall coordination across 12 countries, while a Steering Committee chaired by Prof. David Serwadda provided oversight.
PERSuADE was implemented in two phases between 2018 and 2023. The project brought together 12 universities and 12 Ministries of Health in East and Southern Africa to strengthen analytical capacity and promote data use in national health programmes, cascading skills to districts and lower facilities. In its second phase, the project trained over 1,500 health staff, including 934 at the sub-national level, in data analysis and use, and generated more than 80 analytical outputs on HIV, TB, and malaria. These informed National Strategic Plans in seven countries and improved programme strategies in all 12. Sixteen in-service staff from seven countries received specialised training in HIV key population surveillance, health information systems, and data use. The project also piloted the Maturity Index Model in five countries, helping ministries track progress in institutionalising data-driven decision-making.

In Uganda, the PERSuADE project was implemented in Kiboga, Buikwe, Kasanda, Mukono, and Mityana districts, selected by the Ministry of Health. According to the Principal Investigator, Prof. Rhoda Wanyenze, strengthening data analysis and use has greatly enhanced the capacity of Ministries of Health to deliver targeted interventions that directly benefit communities. She noted that improved analytical skills at national and subnational levels now enable ministries to identify disparities in HIV, TB, and malaria burdens, while district and facility health workers can use data to strengthen local service delivery. “With better data, districts can plan more efficiently, allocate medicines, and implement tailored prevention campaigns to address specific risks, raise awareness, and reduce new infections,” she said, emphasising the role of equitable collaboration as a key success factor in Uganda and across the continent for this partnership.
Indeed, during a learning visit to Uganda in September 2024, Dr. Estifanos Biru Shargie, Senior Specialist for Monitoring, Evaluation, and Country Analysis at the Global Fund, commended the PERSuADE Project for strengthening local capacity and fostering sustainable health system improvements through South-South partnerships among schools and ministries. “The impact has been significant. In Kiboga, I was impressed by how teams mapped gaps in services and addressed them over four years, using data to inform decisions and monitor progress. Working with Makerere University School of Public Health has been an honour. The School blends academic excellence with practical implementation, backed by strong financial management and a long-standing relationship with the Ministry of Health. Their coordination, networking, and efficiency have been exemplary,” Dr. Shargie said.
Another currently ongoing initiative at the School is the African Leadership and Management Training for Impact in Malaria Eradication (ALAMIME) program, led by MakSPH with ten participating institutions across nine malaria-endemic countries, funded by the Bill & Melinda Gates Foundation. Co-led by Prof. Elizeus Rutebemberwa and Prof. Dosithée Ngo Bebe, ALAMIME is cultivating the leadership Africa needs to defeat malaria by strengthening institutions, building capacity, and fostering regional networks. In 2024 alone, the program trained over 250 participants, nearly half women, from national malaria programs, ministries, and NGOs. Through structured training, alumni-led webinars, and cross-country exchanges, the program has demonstrated how equitable, multi-country partnerships translate investment into sustainable systems and shared momentum toward malaria elimination.

For nearly 15 years now, MakSPH has also hosted the NTU–Mak Partnership, a collaboration between Makerere University and Nottingham Trent University, first conceived in 2010, with Assoc. Prof. David Musoke and Prof. Linda Gibson as the Uganda and UK Co-Leads. One of the key reasons for the success of this partnership is equity, and it has since attracted over £1.4 million in grants, trained more than 900 Village Health Teams in Wakiso District, supported over 350 practitioners in antimicrobial stewardship, and facilitated exchanges for more than 200 students and faculty. It has also equipped community health workers to respond to non-communicable diseases, antimicrobial resistance, and the COVID-19 pandemic, while generating over 30 peer-reviewed publications and convening global platforms such as the first International Community Health Worker Symposium, held in Kampala in 2017.
Dr. Musoke, the Co-Principal Investigator for the project on strengthening equitable research collaborations in Uganda, described the NTU-Mak partnership as a model North–South partnership that has produced both joint scholarship and lasting institutional ties. He noted that its success has inspired wider collaborations, as the current project on equitable partnerships builds on this foundation. Emerging from a British Academy regional workshop in Nairobi in 2024, MakSPH extended its engagement to Mountains of the Moon University (MMU), Uganda Martyrs University (UMU), and the National Agricultural Research Organisation (NARO). Together with Nottingham Trent University, these institutions are now advancing reforms to embed equity in research partnerships across Uganda’s research ecosystem.

You may like
-


EfD Uganda Marks 2025 Milestones, Sets Strategic Path for 2025–2029
-


Makerere University Launches Knowledge-Sharing Platform to Drive Innovation and Economic Growth
-


Makerere University CoBAMS Staff celebrate 2025 achievements
-


Makerere University and Tsinghua University Launch Landmark China–Uganda Joint Laboratory on Natural Disaster Monitoring and Early Warning
-


Facilitating Access and Participation through Higher Education Access Programmes and Connected Education for Students with Refugee Backgrounds: A Global South Delphi Study
-


Makerere University Leaders Call for Excellence in Research and Supervision as Academic Staff and PhD Students Receive Certificates
Health
Makerere University and Tsinghua University Launch Landmark China–Uganda Joint Laboratory on Natural Disaster Monitoring and Early Warning
Published
5 days agoon
December 19, 2025
Makerere University has taken a decisive step in strengthening Uganda’s and Africa’s capacity for public safety, disaster preparedness, and climate resilience with the official launch of the China–Uganda Belt and Road Joint Laboratory on Natural Disaster Monitoring and Early Warning, a flagship collaboration with Tsinghua University of China.
Launched during the Makerere University–Tsinghua University Symposium on Public Safety and Natural Disaster Management, the Joint Laboratory positions Makerere as a continental hub for cutting-edge research, innovation, and policy-relevant solutions in disaster risk reduction, early warning systems, and emergency response. The Laboratory will be hosted by Makerere University and is the only facility of its kind in Africa under this cooperation framework, underscoring its regional and global significance.
A Strategic Partnership Rooted in Research, Policy, and Practice
In his opening remarks, Prof. Barnabas Nawangwe, Vice-Chancellor of Makerere University and Ugandan Co-Director of the Joint Laboratory, traced the origins of the partnership to 2018, when a Makerere delegation visited Tsinghua University and the Hefei Institute for Public Safety Research. He recalled being deeply impressed by China’s advanced capacity in public safety research, disaster monitoring, and emergency management capabilities that directly respond to Uganda’s growing exposure to floods, landslides, epidemics, and other hazards.
The Vice-Chancellor noted that the successful establishment of the Joint Laboratory followed a competitive grant process under China’s Belt and Road Initiative, supported by the Government of Uganda and regional partners, including Nigeria and Côte d’Ivoire. He emphasized that the Laboratory aligns squarely with Makerere’s strategic ambition to become a research-led and research-intensive university, while also advancing its internationalisation agenda.

“This Laboratory will significantly enhance Makerere University’s ability to generate evidence-based research that directly informs government policy and public safety interventions. It will serve not only Uganda, but Africa at large,” Prof. Nawangwe said.
He further underscored the Laboratory’s national importance, noting that similar facilities in China are regarded as national-level laboratories, entrusted with supporting government decision-making and national resilience. Relevant Ugandan institutions, including the Office of the Prime Minister (OPM), UPDF, Uganda Police, Ministry of Health, and humanitarian actors, are expected to actively participate in the Laboratory’s work.
Tsinghua University: Advancing Science Diplomacy and South–South Cooperation
Speaking on behalf of Tsinghua University, Prof. Yuan Hongyong, Dean of the Hefei Institute for Public Safety Research and Chinese Co-Director of the Joint Laboratory, described the initiative as both a scientific milestone and a powerful demonstration of South–South cooperation.
He emphasized that natural disasters transcend national borders and demand collective, science-driven responses. By combining Tsinghua’s technological expertise, including satellite monitoring, AI-driven analytics, and integrated early warning systems, with Makerere’s deep regional knowledge and policy engagement, the Joint Laboratory provides a robust platform for innovation, applied research, and practical solutions tailored to African contexts.

The Laboratory will function not only as a research centre, but also as an operational platform for natural hazard monitoring, early warning, risk assessment, and capacity building, supporting Uganda and the wider African region in building more resilient communities.
Government of Uganda: Research as a Pillar of National Resilience
Representing the Office of the Prime Minister, Mr Frederick Edward Walugemba, reaffirmed the government’s strong support for the Joint Laboratory, recognizing research as a cornerstone of effective public safety and disaster management. The OPM highlighted its constitutional mandate to coordinate disaster preparedness and response through institutions such as the National Emergency Coordination and Operations Centre (NECOC).
He mentioned that the Office of the Prime Minister is committed to working closely with Makerere University and its partners, underscoring the importance of multi-agency collaboration, robust data systems, and timely policy advisories to address the complex, multidimensional nature of public safety challenges.
China–Uganda Relations and the Role of Science Diplomacy
Mr. WANG Jianxun, Commercial Counsellor of the Embassy of the People’s Republic of China in Uganda, lauded the Joint Laboratory as a concrete outcome of the growing China–Uganda Comprehensive Strategic Partnership. He emphasized that the collaboration reflects China’s commitment to knowledge sharing, technology transfer, and people-centred development, particularly in areas such as climate adaptation, disaster risk reduction, and sustainable development.
He also highlighted the Belt and Road Initiative as a framework that extends beyond infrastructure to include scientific cooperation, academic exchange, and innovation-driven development, with the Joint Laboratory standing as a model of how universities can advance diplomacy through science.
Makerere’s Multidisciplinary Strength at the Core
In his concluding remarks, Prof. Nawangwe reaffirmed Makerere University’s readiness to operationalize the Laboratory through a multidisciplinary research team spanning public health, geography, engineering, computing, artificial intelligence, social sciences, and the built environment.
He stressed that effective disaster management must integrate technology, human behaviour, governance, and community engagement, noting the importance of sociological insights in addressing risk perception and public compliance during disasters. Makerere will also engage emerging universities and regional partners to ensure the Laboratory’s benefits are widely shared.

The Vice-Chancellor also commissioned an interim, multidisciplinary coordination committee to operationalise the Joint Laboratory, drawing expertise from health, climate science, engineering, artificial intelligence, social sciences, and government agencies.
Hon. John Chrysostom Muyingo Officially Launches the Laboratory
The Joint Laboratory was officially launched by the Honourable John Chrysostom Muyingo, Minister of State for Higher Education, who applauded Makerere University and Tsinghua University for securing the prestigious grant and advancing Uganda’s science and research agenda.

Hon. Muyingo reaffirmed the Government’s commitment to supporting research that informs national development, public safety, and disaster preparedness. He urged Ugandan researchers to fully leverage the partnership to learn from China’s experience in transforming research into actionable solutions for society.
“This Laboratory is a clear demonstration of how strategic international partnerships can strengthen national capacity, inform policy, and protect lives,” the Minister said, as he formally declared the symposium and laboratory launch open.
Positioning Makerere as a Regional Centre of Excellence
Makerere University already plays a critical role in public safety, disaster preparedness, and early warning through a range of research, training, and operational partnerships. Through the School of Public Health (MakSPH) and the Infectious Diseases Institute (IDI), the University has led national and regional initiatives in epidemic preparedness, emergency response, and early warning, including Field Epidemiology Training, risk prediction modelling, and multi-hazard risk assessments that inform district and national preparedness planning. A national assessment of 716 health facilities conducted by MakSPH revealed widespread exposure to climate-related hazards and systemic preparedness gaps, directly informing the Ministry of Health’s Climate and Health National Adaptation Plan (H-NAP 2025–2030)
Makerere has also been at the forefront of disaster risk reduction innovation and community resilience through the Resilient Africa Network (RAN), which has supported scalable, evidence-based solutions such as EpiTent, a rapidly deployable emergency health facility; RootIO, a community-based radio communication platform used for risk communication and early warning; and RIAP Horn of Africa, which advances climate-resilient water harvesting technologies for drought-prone pastoralist communities.

Earlier, the University led the USAID-funded PeriPeri U project (2014–2019) and a disaster management collaboration with Tulane University, strengthening applied research, training, and early warning systems across Africa, efforts that laid the foundation for RAN and Makerere’s current disaster resilience agenda.
In collaboration with government and international partners, Makerere has supported the strengthening of Emergency Operations Centres, including the development of Regional Emergency Operations Centre (REOC) dashboards to improve real-time coordination and situational awareness. IDI has further contributed to epidemic intelligence and early warning, supporting districts to update WHO STAR-based risk calendars, strengthen sub-national preparedness, and enhance real-time decision-making during outbreaks. Makerere teams have also been deployed regionally to support Marburg and Mpox outbreak responses in Rwanda and the DRC, while advancing outbreak modelling as an early warning tool for high-consequence infectious diseases.
Complementing these efforts, the Department of Geography, Geo-Informatics and Climatic Sciences conducts transdisciplinary research on floods, landslides, droughts, soil erosion, and land-use change, using geospatial analysis, earth observation, modelling, and participatory methods to translate complex data into actionable early warning and risk information for policymakers and communities. These ongoing initiatives collectively demonstrate Makerere University’s established capacity in public safety, disaster preparedness, and early warning, providing a strong operational and scientific foundation for the China–Uganda Belt and Road Joint Laboratory.
With strong backing from the Governments of Uganda and China, as well as leading international partners, the China–Uganda Belt and Road Joint Laboratory on Natural Disaster Monitoring and Early Warning is poised to become a regional centre of excellence for disaster risk reduction research, training, and innovation.
The Laboratory will contribute to improved early warning systems, faster emergency response, stronger policy coordination, and enhanced scientific capacity, cementing Makerere University’s role at the forefront of addressing some of the most pressing public safety challenges facing Uganda, Africa, and the global community.
Caroline Kainomugisha is the Communications Officer, Advancement Office Makerere University.
Health
Makerere University Explores Strategic Partnership with Tsinghua University in Safety Science, Disaster Resilience and Public Health
Published
1 week agoon
December 16, 2025
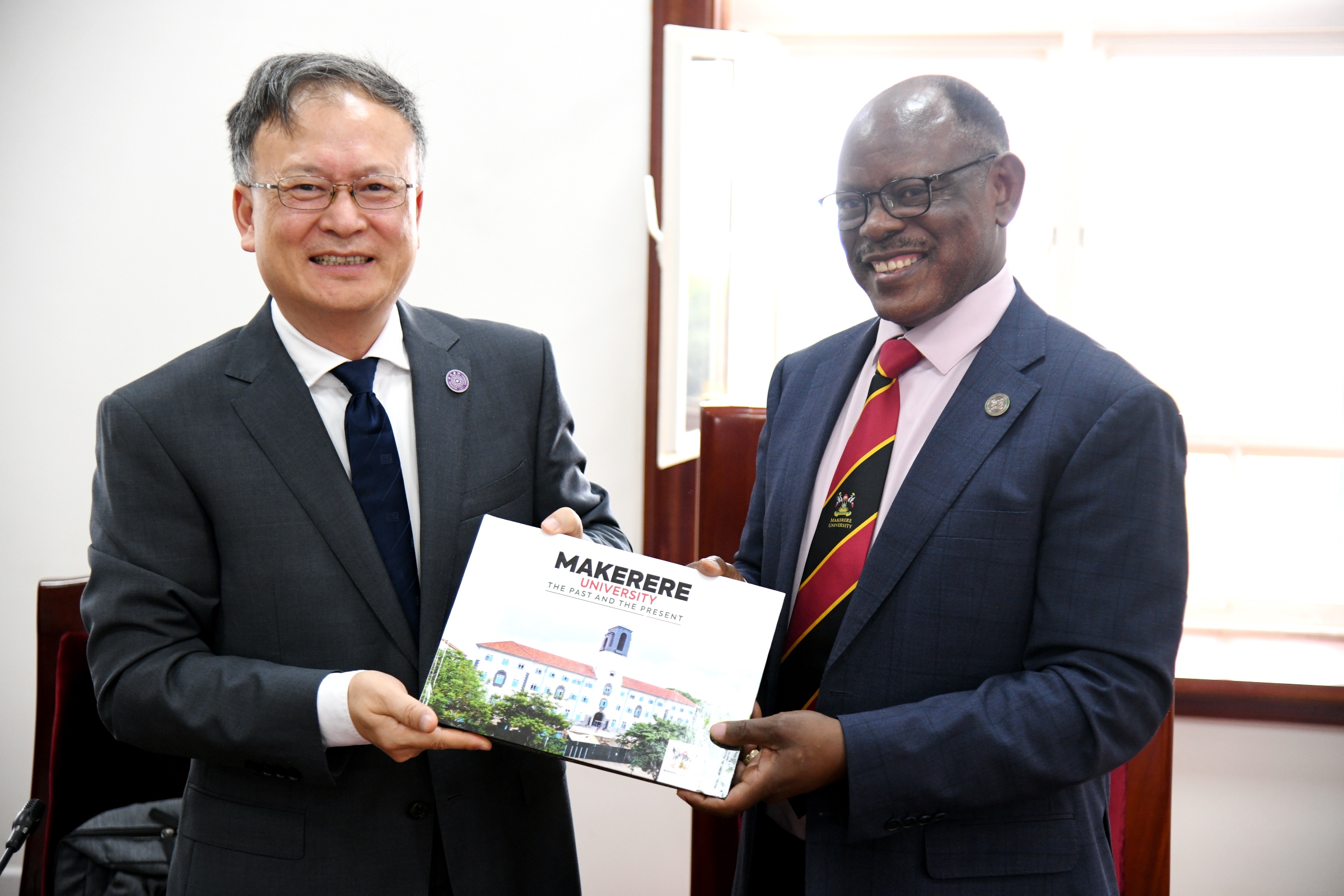
Makerere University has taken a significant step toward strengthening global research collaboration following a high-level meeting between Vice Chancellor Prof. Barnabas Nawangwe and a delegation from Tsinghua University’s Hefei Institute for Public Safety Research, one of China’s leading centres of excellence in disaster prevention, public safety, and emergency management. The engagement marked a renewed commitment to advancing scientific cooperation between the two institutions, particularly in addressing complex environmental and public health challenges that continue to shape national and global development.
A Partnership Anchored in Shared Challenges and Global Priorities
In his remarks, Prof. Nawangwe emphasized that the concept of comprehensive public safety, spanning natural disasters, epidemics, infrastructure failures, and social risks, is increasingly relevant to all colleges and disciplines at Makerere. Uganda’s experience with epidemics such as Ebola, cholera, and COVID-19; frequent landslides in mountainous regions; flooding events; and rising traffic-related incidents place the University in a unique position to contribute applied research, community-based insights, and local knowledge to a global scientific dialogue.
He noted that the Tsinghua presentation revealed new areas of alignment, particularly in epidemic modelling, early-warning systems, and integrated emergency management, areas where Makerere’s public health scientists, medical researchers, and social scientists have extensive expertise.
“This collaboration offers meaningful opportunities for nearly every college at Makerere,” he noted. “Public safety touches the environment, public health, engineering, social sciences, ICT, humanities, and urban planning. The challenges we face as a country make this partnership both timely and essential.” Prof. Barnabas Nawangwe noted.
Tsinghua University: A Global Leader in Comprehensive Public Safety.
The delegation from Tsinghua University outlined China’s national investment in Public safety over the past two decades, an effort driven by the recognition that life and security are the foundation of sustainable development. Tsinghua’s Hefei Institute for Public Safety Research has developed nationally recognised research platforms and large-scale simulation facilities dedicated to Natural disaster modelling (earthquakes, landslides, floods, typhoons, Infrastructure and urban systems safety, Public health emergencies and epidemic preparedness, Early-warning, monitoring, and emergency communication, Traffic and transportation safety, Post-disaster reconstruction and resilience planning.
Their systems currently support over 100 provincial and municipal emergency management centres in China, underscoring their global leadership in practical, scalable solutions for disaster risk management. The delegation reaffirmed that Uganda’s lived experience with multiple hazards presents opportunities for meaningful knowledge exchange. They expressed particular interest in learning from Makerere’s work on epidemic response, community health systems, and the social dimensions of disaster management.
Emerging Areas of Partnership
The meeting identified several promising pathways for long-term collaboration:
1. Joint Research in Disaster Risk Reduction and Climate-Related Hazards
Both institutions expressed readiness to co-develop research projects on landslides, floods, urban resilience, and multi-hazard modelling, drawing on Tsinghua’s advanced simulation technologies and Makerere’s environmental expertise and geographic field realities.
2. Public Health Emergency Preparedness and Epidemic Response
Makerere’s renowned public health schools and research centres will collaborate with Tsinghua on epidemic prediction, early-warning systems, and integrated preparedness frameworks, leveraging Uganda’s decades of experience managing high-risk disease outbreaks.

3. Infrastructure and Urban Safety, Including Traffic Systems
With Uganda experiencing rapid urbanisation and high rates of motorcycle-related road incidents, Tsinghua shared insights from China’s own transformation, including infrastructure redesign, transport modelling, and public transit innovations. Collaborative work in this area would support city planning and road safety interventions in Kampala and other urban centres.
4. Academic Exchange and Capacity Building
Both sides expressed interest in student exchanges, staff mobility, co-supervision of postgraduate research, and specialised training programmes hosted at Tsinghua’s world-class safety research facilities.
5. Development of a Joint Public Safety Laboratory at Makerere
The institutions are exploring the establishment of a collaborative safety research platform in Uganda. This initiative could serve as a regional hub for innovation in emergency management, environmental safety, and technology-driven risk assessment.
Towards a Long-Term, Impactful Collaboration
The meeting concluded with a shared commitment to develop a structured partnership framework in the coming months, supported by both universities and aligned with Uganda–China cooperation priorities. Both teams acknowledged that the partnership must yield tangible results that enhance community resilience, bolster national preparedness systems, and foster scientific capacity for future generations.
Prof. Nawangwe commended Tsinghua University for its willingness to co-invest in research and capacity building, noting that such collaborations position Makerere not only as a leading research institution in Africa but as an active contributor to global scientific progress.

“This partnership has the potential to transform our understanding of the science of public safety to deliver solutions that safeguard lives.” Prof. Barnabas Nawangwe noted.
“It aligns perfectly with Makerere’s mission to be a research-led, innovation-driven university responding to the world’s most urgent challenges.” He added.
As part of this strategic partnership engagement, Makerere University will, on Wednesday, 17th December, co-host the Makerere University–Tsinghua University Symposium on Public Safety and Natural Disaster Management. The symposium will run from 8:00 AM to 2:00 PM in the University Main Hall, Main Building.
This symposium represents a deepening of collaboration not only between Makerere University and Tsinghua University, but also a broader strategic partnership between Uganda and the People’s Republic of China.
During the event, H.E. Zhang Lizhong, Ambassador of the People’s Republic of China to Uganda, together with the State Minister for Higher Education, Government of Uganda, will officially launch the China–Uganda Belt and Road Joint Laboratory on Natural Disaster Monitoring and Early Warning. The Laboratory will be hosted at Makerere University, positioning the University to play a central role in strengthening Uganda’s and the region’s capacity for natural disaster preparedness, public safety, and emergency management research.
Caroline Kainomugisha is the Communications Officer, Advancement Office, Makerere University.
Health
Three Years of Impact: Makerere University Health User Committee Presents Status Report
Published
2 weeks agoon
December 12, 2025By
Eve Nakyanzi
Makerere University on 11th November 2025 marked a significant milestone as the Health User Committee (Mak-HUC)—established by the Vice Chancellor in 2022 as part of his strategic mandate to strengthen and oversee the University’s health service delivery—formally handed over its three-year report. The event highlighted the committee’s achievements in guiding, monitoring, and improving Makerere University Health Services, presenting a record of progress that has reshaped confidence, strengthened systems, and expanded care for staff and students.
A Call for Integrated and Sustainable Health Services
The Vice Chancellor Prof. Barnabas Nawangwe emphasized the need for a more integrated, efficient, and sustainable approach to delivering health services for Makerere University staff and students. He noted that while the University does not receive supplies from the National Medical Stores system, its community remains entitled to quality care, urging renewed consideration of how essential services—such as drug access, surgical limits, and special medical cases—can be better supported. He highlighted the importance of practical costing models, especially for extending care to staff dependents, and called for flexibility in managing exceptional cases like complex surgeries or referrals abroad.

The Vice Chancellor also underscored the urgent need to modernize the University Hospital, proposing that Makerere begin incrementally establishing a teaching hospital using existing facilities and leveraging expertise of highly qualified consultants the College of Health Sciences (CHS). He reiterated that government budget ceilings remain a major constraint, but encouraged the committee to develop a concept that could be presented to Council and later supported through strategic engagement with the Ministry of Finance, Planning and Economic Development. Throughout his remarks, he applauded the Mak-HUC for its work and reaffirmed that even with the creation of a professional hospital board, the committee must remain central in representing service users.
Aligning Health Services with Sustainable Insurance Models
Prof. Bruce Kirenga the Principal College of Health Sciences responded by clarifying the committee’s efforts to align Makerere’s health services with real insurance models, including cost projections for covering additional family members and encouraging voluntary staff contributions where necessary. He acknowledged the complexity of expanding service coverage—especially in cases of chronic illness or high-cost procedures—but emphasized the committee’s commitment to cautious, sustainable planning. He confirmed that the College is working closely with the Hospital to improve services, attract specialists, and integrate students into the health system, a model that naturally draws academic staff into clinical roles without imposing unrealistic obligations.

Prof. Kirenga also noted the College’s ongoing assessments of facility needs, including dialysis, ICU expansion, and equipment placement, stressing that the ultimate goal is a unified, well-structured health network across the University. He welcomed the Vice Chancellor’s support for transforming existing facilities into a teaching hospital and pledged to refine proposals that reflect both current realities and long-term institutional needs.
Committee Chair Reflects on Three-Year Achievements
Dr. Allen Kabagyenyi, Chair of Mak-HUC, reflected on the three-year journey with gratitude and pride, noting that the committee not only fulfilled its terms of reference but exceeded expectations. She highlighted major gains made under the Vice Chancellor’s support, including transforming the University Hospital into a self-accounting unit—an intervention that unlocked smoother financial management and accelerated service delivery. Dr. Kabagyenyi commended the strong collaboration with the Hospital administration, Human Resources Directorate, and other units, which ensured staffing stability even during institutional transitions.

She pointed to the expansion of referral partnerships—now totaling 29 health facilities nationwide—as a crucial achievement that guarantees continuity of care for staff and students wherever they are. She also emphasized the committee’s work in guiding policies for specialized treatment and cross-border care, strengthening fraud-prevention systems, and advancing digital transformation through an integrated health information system and the new Makerere University Health Services (MakHS) website. Dr. Kabagyenyi noted that these improvements have directly benefited staff and enhanced the overall quality of care, supported by close collaboration with the College of Health Sciences and access to some of the country’s best consultants. She concluded by underscoring the ongoing need for a comprehensive University Health Policy and expressed deep appreciation to the Vice Chancellor and University Management for their unwavering openness and support—attributes she credited for the committee’s success.
Highlights of Service Growth and Infrastructure Upgrades
The Chief, Makerere University Health Services, Prof. Josaphat Byamugisha, highlighted the significant progress achieved under the Health User Committee’s oversight, noting especially the steady rise in service utilization and renewed confidence among staff and students. He emphasized that trust in the University Hospital has grown organically—built not through advertising, but through improved patient experience, stronger systems, and word of mouth.

Prof. Byamugisha pointed to major achievements such as expanded Out-Patient Department (OPD) attendance, better student access to care, enhanced infrastructure including modernized theatres capable of complex procedures, and upgraded laboratories supported through framework agreements that ensure continuous equipment renewal. He noted that specialized clinics, increased inpatient capacity, and expanded referral networks have strengthened the Hospital’s reach and responsiveness. The Hospital is also taking on more research work and clinical training, partnering with units such as optometry, internal medicine, and the Clinical Trials Unit, with new collaborations—like the MasterCard Foundation—driving further growth.
He reaffirmed that the long-term vision of establishing a fully-fledged Makerere University Teaching Hospital is taking shape through coordinated efforts with the College of Health Sciences. Prof. Byamugisha credited the Vice Chancellor’s support for enabling these strides and expressed deep appreciation to all stakeholders contributing to the continued improvement of health services for the entire University community.
DICTS Unveils Modular Information System & Health Services Website
The Directorate for ICT Support (DICTS) presented the newly developed Makerere University Integrated Health Management Information System (MakIHMIS), designed around a modular system that streamlines all hospital processes. The platform integrates eight functional modules, including registration, triage, clinician workflows, inventory and medicines management, pharmacy dispensing, laboratory information management, user management, and linkages to both the Academic and Human Resource Management Information Systems ACMIS and e-HRMS respetively. Most of these modules are already active, enabling smooth patient registration, accurate record-keeping, real-time inventory tracking, and seamless access to student and staff data without duplication. Only two modules—land and insurance—remain under development before the system becomes fully end-to-end. The MakHS website on the other hand features information about hospital services, events, research activities, and staff profiles, offering both the university community and the public a centralized and efficient digital gateway to the hospital’s operations.

The term of the outgoing committee has officially concluded, and preparations are now underway for the incoming committee to assume its duties and continue advancing the work ahead.
Trending
-

 Research4 days ago
Research4 days agoMakerere University Launches Knowledge-Sharing Platform to Drive Innovation and Economic Growth
-

 General6 days ago
General6 days agoMakerere University Leaders Call for Excellence in Research and Supervision as Academic Staff and PhD Students Receive Certificates
-

 Humanities & Social Sciences2 weeks ago
Humanities & Social Sciences2 weeks agoCollege of Humanities and Social Sciences Launches Five Groundbreaking Publications
-

 Health2 weeks ago
Health2 weeks agoThree Years of Impact: Makerere University Health User Committee Presents Status Report
-

 Health1 week ago
Health1 week agoMakerere University Explores Strategic Partnership with Tsinghua University in Safety Science, Disaster Resilience and Public Health
