Health
Uganda Newborn Programme Shifts the Paradigm of Newborn Care
Published
11 months agoon
By
Mak Editor
By Joseph Odoi
Every newborn deserves the best start to life. Yet, in Uganda, the burden of newborn morbidity and mortality remains high. The newborn mortality rate stands at 22 deaths per 1000 live births (UDHS 2022). According to most recent UN annual estimates, Uganda records 62,000 deaths around the time of birth. Of these, 32,000 are neonatal deaths, 26,000 are stillbirths and 4,800 are maternal deaths. Majority of the newborn deaths occur within the first week after delivery- a period considered very vulnerable for both the mother and baby.
Uganda’s high fertility rate translates to about 1.7 million births per year; and of these 250,000 babies need special newborn care as they are either born too small or fall sick within the first month of life. This has placed a huge burden on the country and strained the already limited investment for neonatal care.
Despite national efforts, newborn deaths continue to account for nearly half of all under-five deaths in Uganda, according to the Uganda Demographic and Health Survey (UDHS) 2022.
To contribute to addressing this challenge, a coalition of institutions namely; Makerere University School of Public Health, Baylor Foundation Uganda, Adara Development Uganda, Nsambya Hospital, and the Ministry of Health with funding from ELMA Philanthropies launched a national health systems strengthening initiative known as the Uganda Newborn Programme (UNP) in 2022. This program uses a regional approach to improve newborn care in three regions of Uganda namely Kampala, North Central and Western regions.
According to Dr. Monica Okuga, the Uganda Newborn Programme Coordinator at Makerere University School of Public Health (MakSPH), the Uganda Newborn Programme (UNP) made huge strides in providing quality newborn care in 36 health facilities across the three regions of Uganda.
Uganda New Born Programme Achievements
‘’Under the UNP, there have been so far many achievements. Institutional neonatal mortality rate has reduced in the facilities where the program is implemented and this has contributed to overall reduction in neonatal mortality in the regions. For example, Institutional neonatal mortality reduced to 7/1000 and 2/1000 live births by the end of Year 2, down from the baseline rates of 8.4/1000 and 11.9/1000 in Bunyoro and Tooro, representing reductions of 16.7% and 85.3% respectively’’ Dr. Okuga stated.

Dr. Okuga further explained that, ‘’Overall asphyxia case fatality rates across program areas have also reduced from 8.9% to 5%; adherence to infection prevention and control measures has improved across the facilities; and the quality of newborn care provided has also improved.
In addition to revamping many newborn care units, Dr. Okuga revealed that the programme supported the construction of newborn care units, citing Kyegegwa Hospital, Buliisa General Hospital, Masindi General Hospital, and Kyangwali HCIV.
In line with the SDGs programme objectives, specifically SDG 3; Good Health and Well-Being, Makerere University School of Public Health, together with partners including the National Planning Authority (NPA), UNICEF, FHI360, and the Ministry of Health, produced the Situation Analysis of Newborn Health in Uganda-2023 update.
This document has now been taken up by the Ministry of Health and is being used to develop a strategy for implementing the suggested recommendations therein, as well as costing the investment for improving newborn health in Uganda.
The previous newborn situation analysis was conducted 17 years ago in 2008’’ she explained of programme contribution at a multi-sectoral level

Establishment of Uganda’s First Breast Milk Bank
Still under this programme, the first ever Breast Milk bank was established at Nsambya hospital with other donor milk satellite sites at Mengo, Rubaga, Kibuli and Naguru hospitals in Kampala. This donor breast milk has benefited over 275 babies across Kampala and its neighboring districts.

Hospital-to-Home (H2H) Initiative
Another innovation that has been scaled up through the programme is the Hospital to Home (H2H) initiative by Adara Uganda. While many newborn interventions focus primarily on in-hospital care, the Uganda Newborn Programme, in partnership with Adara Development Uganda, pioneered the Hospital-to-Home (H2H) Model, extending its newborn care continuum to the household level. This innovative model ensures that high-risk newborns continue to receive vital support after hospital discharge, addressing the gaps in follow-up care that are common in low-resource settings.
According to Beatrice Niyonshaba, Deputy Director of Maternal, Newborn, and Child Health at Adara Development; “In Uganda, many families struggle to return for follow-up visits due to cost, transport challenges, and lack of caregiver awareness. The H2H model addresses this by involving caregivers early, equipping them with knowledge on newborn danger signs, and ensuring post-discharge follow-up through community health systems like village health teams.”

She adds, “The model not only reduces post-discharge mortality but also builds trust and ownership among families, which is critical but often an overlooked aspect of newborn survival in low-income settings. ‘’We also run regular community sensitization and awareness initiatives about the causes and survivability of small and sick newborns, preventative measures, as well as the services”. The model was initially piloted at Kiwoko Hospital, with strong support from both healthcare staff and the community. This phase allowed for continuous refinement and strengthening of the model, ensuring it met the needs of both families and healthcare providers.’’ Ms. Niyonshaba explained of the H2H Model uniqueness

Currently, the model is being implemented in Nakaseke hospital, a government facility. This will provide insights for scale up to other government facilities. The programme has seen tremendous success due to the engagement and motivation of CHWs, who are provided with incentives, extensive training, and ongoing support. Regular check-ins and monthly meetings ensure these workers remain accountable and connected to the Programme’s objectives.
Challenges in Newborn Care
According to Dr. Monica Okuga and Prof. Peter Waiswa, the Uganda Newborn Programme team lead from MakSPH, in spite of the many achievements, several challenges persist. They explain that many health facilities in Uganda were built without infrastructure to support Newborn Care Units (NCUs). There are no standard floor plans for these units. In many facilities, the neonatal care units are housed in improvised rooms, while in some cases, completely new NCUs are built.
However, even where NCUs are present, they are often let down by an unstable power supply, despite the fact that most equipment in the NCUs require consistent electricity to function. In addition, there are other health system challenges such as insufficient drug supplies from the government, inadequate staffing, and the low involvement of medical officers in neonatal care. Internal rotation of already trained nurses to other units further worsens the situation. Other issues include untimely or late referrals of mothers and babies, as well as challenges with the low quality of data produced in these units.
In terms of lessons learnt while implementing the UNP, The Uganda Newborn Programme team observed and noted several key lessons during the implementation of the programme
- The importance of leadership engagement in the uptake of interventions is very critical. The leaders to be engaged not only include those at the facility level but also those at the district level. The support of political district leaders such as the Chief Administrative Officer (CAO) is also very crucial. One way of engagement is through sharing performance dashboards with key indicators to the District Health Officers (DHOs), CAO, and Health Facility In-charges.
- There is a need for continuous engagement of district leadership for sustainability in public health facilities, especially the human resource aspect for established Newborn Care Units (NCUs).
- There is a need to intervene across the board/spectrum of the health system. Addressing one challenge, for example, the provision of equipment, may not result in the required benefits without addressing human resources and skills.
- Using a regional approach to care, which includes all hospitals and high-volume health centres, is a more rapid and cost-effective way to scale up maternal and newborn care. It also improves access, quality, and referral, thus reducing unnecessary mortality.
- Regional Local Maternity and Neonatal Systems (LMNS) provide avenues/platforms to share lessons and share feedback to teams/facilities on gaps identified.
- Targeted mentorships not only maintain skills but also support teams in innovating for problem-solving.
- Continuous engagement of medical officers in facilities creates buy-in and brings them on board to support and bridge gaps in newborn care in the neonatal care units.
In terms of sustainability, the team stated that the programme’s design took into account the potential for continuation beyond the initial funding from ELMA Philanthropies. From the outset, the Ministry of Health was actively involved in the co-creation of the programme. The programme also made effective use of existing staff and infrastructure to enhance the quality of newborn care. While there was occasional catalytic provisions of drugs and equipment, the programme primarily relied on the government’s drug supply and delivery systems to ensure long-term sustainability.
About The Uganda Newborn Programme (UNP)
The Uganda Newborn Programme (UNP) has been actively working since its launch in July 2022, with the goal of significantly improving the care for small and sick newborns across the country. With support from ELMA Philanthropies, the programme has brought together a consortium of partners, including Makerere University School of Public Health, Baylor Uganda, Adara Uganda, and Nsambya Hospital, in collaboration with the Ministry of Health.
The programme is focusing on 20 high-burden districts across three regions of Uganda ie Western, Kampala, and North-Central, serving approximately 1.5 million births annually. Since its inception, the programme has been making strides in enhancing the capacity of health facilities, including the refurbishment and equipping of 30 specialized neonatal care units. These units are designed to meet the needs of small and sick newborns, in line with the National Essential Newborn Care (NEST) Toolkit.
Key activities that have been rolled out include
- Training and mentorship of Health Workers; More than 800 health workers have been trained and mentored in essential neonatal care practices such as neonatal resuscitation, Kangaroo Mother Care (KMC), Continuous Positive Airway Pressure (CPAP), and infection prevention and control. This has significantly improved the clinical competencies of healthcare providers in the management of small and sick newborns.
- Strengthening Infection Prevention and Control; The programme has focused on improving infection control measures at hospitals, which is critical in managing the high rates of sepsis and other infections among newborns.
- Effective implementation of newborn resuscitation and warm transport: This includes establishing standardized protocols and providing essential equipment like mabu bags plus masks, CPAP machines
- Improving Data Utilization; Efforts have also been made to ensure that health workers are using data-driven evidence for decision-making. Monthly perinatal death audits and support for data quality review have allowed for continuous improvement in service delivery.
- Enhanced Postnatal Care; Community-based postnatal care using Village Health Teams (VHTs) being trained to conduct home visits for newborns discharged from neonatal units. This helps ensure that infants receive timely follow-up care in the critical days after discharge.
The programme is set to run up to July 2025, and by then, it aims to have reached 120,000 small and sick newborns, helping to reduce newborn mortality by 40% in the target regions.
You may like
-


Over 9,200 to graduate at Makerere University’s 76th Graduation
-


76th Graduation Highlights
-


Meet Najjuka Whitney, The Girl Who Missed Law and Found Her Voice
-

Makerere University School of Public Health Graduates First Cohort of Cost-Effectiveness Analysis Short Course
-

Climate variability found to shape malaria trends in Yumbe District
-


Mak hosts First African Symposium on Natural Capital Accounting and Climate-Sensitive Macroeconomic Modelling
Health
Makerere University School of Public Health Graduates First Cohort of Cost-Effectiveness Analysis Short Course
Published
4 days agoon
February 20, 2026By
Mak Editor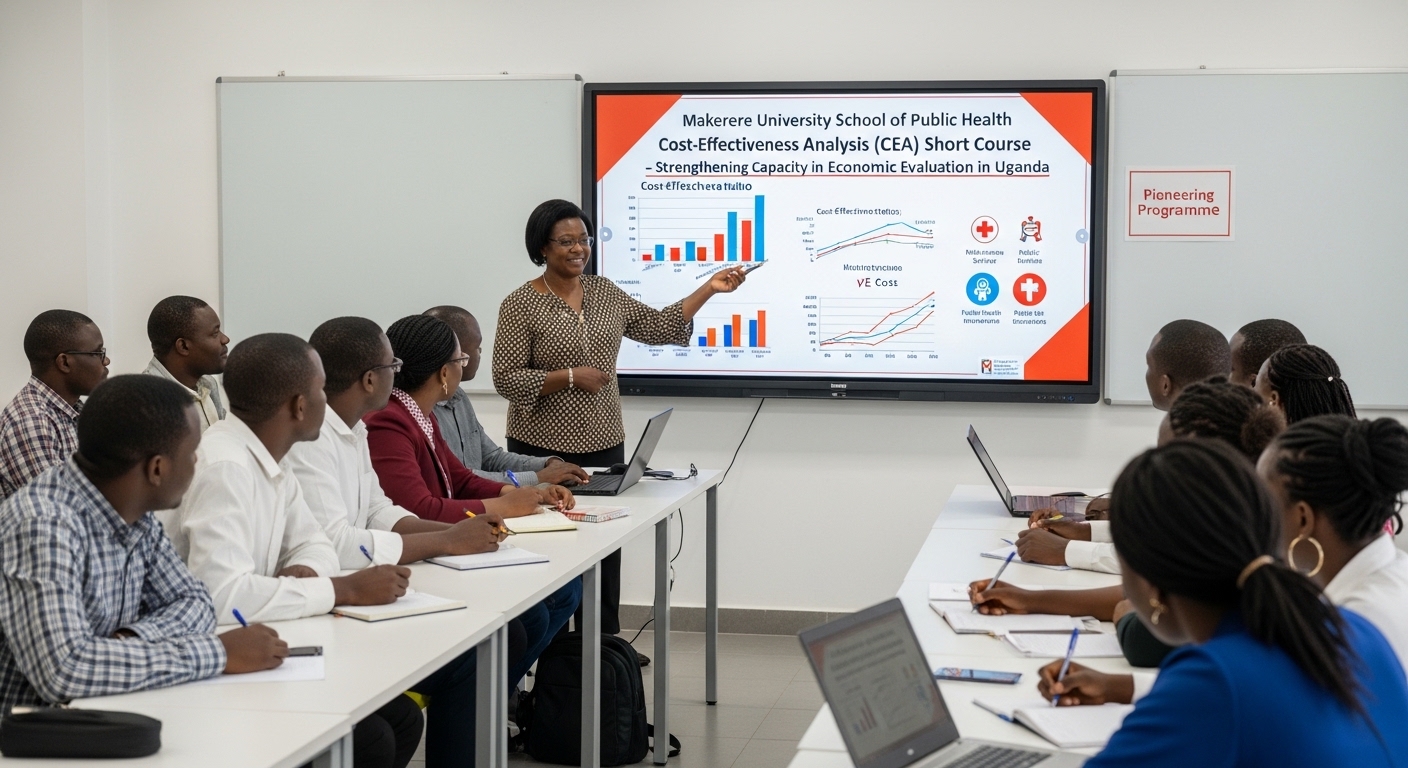
Kampala, Uganda – The Makerere University School of Public Health (MakSPH) has marked a significant milestone with the graduation of the first-ever cohort of its Cost-Effectiveness Analysis (CEA) Short Course. The pioneering programme is designed to strengthen capacity in economic evaluation in Uganda and beyond.
The virtual graduation ceremony honored eleven (11) participants who completed the course. The cohort included professionals from academia, research institutions, government agencies, and non-state actors, reflecting the increasing demand for skills in economic evaluation across sectors.
The short course was developed and implemented by the Department of Health Policy, Planning, and Management (HPPM) in response to the increasing need for evidence-informed decision-making in a context of limited resources.
In her remarks during the ceremony, Assoc. Prof. Suzanne Kiwanuka, Head of the Department of Health Policy, Planning and Management (HPPM) at MakSPH, congratulated the inaugural cohort for completing what she described as a “critical and timely” course.
“With decreasing resources and rising demand for services driven by population growth and the emergence of high-cost technologies, decision-makers must make difficult choices,” she noted. “Cost-effectiveness analysis is no longer optional. It is central to conversations in the corridors of power.”
The CEA short course was designed to equip policymakers, researchers, and practitioners with both theoretical knowledge and practical skills in economic evaluation. Participants were introduced to key principles of health economics, costing methodologies, decision-analytic modelling, Markov modelling, sensitivity analysis, and interpretation of incremental cost-effectiveness ratios (ICERs).
According to Prof. Elizabeth Ekirapa, the course lead at MakSPH, this inaugural offering had been “a long time coming,” following years of discussions within the department about building local expertise in economic evaluation.
Delivered over 10 days through interactive online sessions, the course combined lectures, case studies, and hands-on modelling exercises using contextually relevant datasets. Participants were required to develop and present applied cost-effectiveness projects as part of their assessment, allowing them to translate theory into practice.
During the feedback session at the graduation ceremony, faculty emphasized the importance of clarity in defining study perspectives, selecting appropriate outcomes, and aligning research questions with modelling approaches.
Dr. Chrispus Mayora, one of the facilitators, highlighted the need to carefully select outcomes that directly reflect the intervention being evaluated. “When thinking about outcomes, ask yourself: Is this aligned with what I want to study? Interesting outcomes are not always the most appropriate ones,” he advised.
Participants were also encouraged to select modelling techniques such as decision trees or Markov models based on the research question and the nature of the disease or intervention under study.
Prof. Ekirapa described the graduates as “trailblazers,” noting that their feedback would shape future iterations of the course. “When you are the first cohort, you are like pioneers,” she remarked. “We are committed to improving this course to ensure it becomes a world-class programme.”
For many attendees, the graduation ceremony was a new experience, as certificates were awarded virtually an approach that participants welcomed as innovative and inclusive.
“Cost-effectiveness analysis enables us to maximise value for money,” noted Dr. Crispus Mayora of MakSPH. “It allows decision-makers to compare interventions systematically and ensure that limited resources achieve the greatest possible benefit.”
The programme aligns with Makerere University’s broader mandate to provide high-quality training that responds to national and regional development priorities. Participants who successfully complete the course receive a certificate signed by the Dean of the School of Public Health.
As the ceremony concluded, faculty encouraged continued engagement beyond the classroom. Graduates were urged to refine their project ideas and collaborate with the department in advancing research and policy discussions.
The successful completion of the first CEA short course marks an important step in building a cadre of professionals equipped to conduct rigorous economic evaluations. With plans to expand and refine the programme based on participant feedback, the HPPM department under MakSPH is positioning itself as a regional leader in health economics and policy analysis training.
Health
Uganda has until 2030 to end Open Defecation as Ntaro’s PhD Examines Kabale’s Progress
Published
6 days agoon
February 18, 2026
Silhouettes slip along narrow paths, farmers heading to their gardens, women balancing yellow jerrycans on their hips, children in oversized sweaters hurrying to school, and herders steering cattle toward open pasture, each movement part of a choreography older than memory. This is a quiet ritual in Kabale’s terraced hills, moments before the sun lifts.
The quiet procession to ahakashaka, or omukishaka, often sees figures moving quickly along familiar footpaths in the half-light, as children and adults walk with the urgency of habit. It is not a stroll but often a small, hurried run before daylight exposes what should be private.
It is February 2026, and the century-old Makerere University is celebrating its 76th Graduation Ceremony. The world paces and races toward artificial intelligence and digital revolutions. But some families still begin their day by rushing to the bushes for relief and concealment, while others engaged in economic activities such as gardening and grazing have no sanitation option other than using their surroundings to respond to the nature call!
The deadline to end open defecation is 2030. The science is settled, and the commitments are written into Sustainable Development Goal 6. Yet in parts of Kabale, only a small fraction of households is truly open defecation free.
In his PhD research, Dr. Moses Ntaro did not start with global targets or conference declarations. He began where the morning run ends, at the edge of the compounds, behind banana stems, along worn paths leading to Omukishaka. He asked whether students, equipped not with bricks but with conversation, follow-up, and persistence, could help communities replace that dash with something quieter: a door that closes.
What he found is both hopeful and unsettling. Change is possible. But dignity, like sunrise, should not require a run. And with 2030 approaching, time is no longer generous.

The Question That Would Not Let Him Go
Ntaro did not encounter open defecation as a statistic. While on foot and serving as Assistant Coordinator of Community-Based Education at Mbarara University of Science and Technology (MUST), he learned while supervising students placed in rural communities across southwestern Uganda. They walked villages together, conducted transect walks… and they observed.
“In my role as academic coordinator,” he explains, “students always took me on transect walks within the villages to show me how high open defecation practice was. The effect was evident in the high prevalence of intestinal infections we saw in health facility records.”
The link between sanitation and disease was not theoretical but visible in clinic registers. Diarrhea, intestinal worms, recurring infections among children, and more were all visible in the clinic registers.
Nineteen years ago, in 2007, Uganda adopted Community-Led Total Sanitation (CLTS), a strategy designed to trigger collective behavior change and eliminate open defecation. Progress, however, remained uneven. That same year, Ntaro was working as an Environmental Health Officer with the Water and Sanitation Development Facility under the Ministry of Water and Environment. He was three years away from completing his Environmental Health degree at Makerere University School of Public Health.
And so, the question emerged, to Ntaro, that, ‘If students are already embedded in these communities through COBERS placements, why are we not intentionally harnessing them to accelerate sanitation change?’
That question became his PhD.

This is a Crisis That Should No Longer Exist
Globally, more than 350 million people still practice open defecation. Sub-Saharan Africa carries a disproportionate share. SDG 6, specifically Target 6.2, commits the world to ending open defecation and ensuring universal access to safe sanitation and hygiene by 2030. It prioritizes women, girls, and vulnerable populations. It speaks of dignity, of safely managed services, and of disease prevention.
We are four years away from that deadline. And in rural Kabale District, somewhere in southwestern Uganda, Ntaro’s research found that only 3 percent of households were truly open defecation-free.
Yes, three percent. His 2025 BMC Public Health study examined 492 residents. The average age was 49. Nearly 30 percent had no formal education. Most were women, the custodians of household hygiene and child health.
The determinants of Open Defecation Free (ODF) status were deeply behavioral.
Male-headed households had higher odds of being ODF. Households with clean compounds, clean latrine holes, and consistent handwashing practices were significantly more likely to sustain sanitation improvements.
Sanitation, Ntaro realized, is not only infrastructure but also power, memory, habit, and social expectation.
“Factors associated with ODF status were not just economic,” he notes. “They were behavioral and contextual.”

Why It Feels So Wrong to Still Discuss This
Talking about open defecation in 2026 feels unsettling for three reasons. First, it feels like a failure of basic dignity.
Think of an era of global connectivity and rapid technological advancement, and hundreds of millions still lack privacy. For women and girls, this exposes them to harassment, exploitation, and fear. Sanitation is not just about disease but safety.
Second, it feels like an avoidable health crisis. One gram of feces can contain millions of viruses, bacteria, and parasites. Open defecation directly fuels cholera, typhoid, diarrhea, and environmental enteropathy, a silent contributor to child malnutrition and stunting. The science is settled, and yet the practice persists.
Third, it feels like a poverty trap. Illness leads to lost productivity; lost productivity deepens poverty, and poverty limits investment in sanitation. The cycle continues.
“Open defecation is not simply a sanitation issue,” Ntaro says. “It is linked to poverty, nutrition, and broader development.”

Testing a Different Approach
Ntaro’s doctoral thesis, “Effect of Student Community Engagement on Open Defecation-Free Status,” tested whether health profession students could effectively facilitate Community-Led Total Sanitation.
In some villages, traditional Health Extension Workers led the sanitation process. In others, trained students facilitated it under the COBERS (Community-Based Education, Research, and Service) model, which places medical trainees in community health facilities to learn through real-world practice, bridging classroom theory with primary care and public health work in rural settings.
Through this model, students led triggering, follow-ups, and community engagement. Open defecation declined. More households achieved Open Defecation Free status. And the cost per household was lower than in traditional approaches.
“Students were more effective,” Ntaro explains. “More households became open defecation-free compared to the traditional approach. And they were a cheaper human resource.”
But cost was not the real breakthrough. Presence was. Students stayed for weeks. They returned to check on latrines. They built trust. They kept coming back. Because sustainability, Ntaro argues, is not built in a single visit. It is built in repetition.
“There is a need for continued follow-ups and continued student engagement if long-term impact is to be realized.”
Change cannot be declared once and forgotten.

Behavior… and Not Just Bricks
Using the RANAS framework, Ntaro found that households that remembered to wash hands and kept latrines clean were far more likely to sustain Open Defecation Free status. In sanitation, behavior leaves evidence.
“Behavioral change interventions that empower communities,” he recommends, “such as CLTSH, should be strengthened to increase households with ODF status.”
In other words, building latrines is not enough, but communities must believe in them.

The Defense and the Countdown
On December 11, 2025, Ntaro defended his PhD. Examiners pressed him on scale and sustainability. Could student engagement be institutionalized? Could universities be embedded in district sanitation planning?
His answer was pragmatic: “Yes, but community-based education must be included in planning and budgeting.”
Four years remain to meet SDG 6.2. Four years to end open defecation and turn dignity from promise into practice. In 2026, this conversation should feel outdated. Instead, it remains urgent.

The Slow Work of Restoration
In Kabale, progress does not look dramatic. It looks like a latrine door closing firmly behind someone, a handwashing station with water and soap, a compound swept clean. It looks like a child who does not fall ill this month. Public health victories are often quiet.
As Makerere University approaches its 76th Graduation Ceremony, Dr. Ntaro Moses stands among its PhD graduands not with theory alone, but with evidence that change can be accelerated by reimagining who leads it. Students, he shows, are not only learners. They are the workforce, facilitators, and bridges between policy and path.
The hills of Kabale still wake under mist. But in more compounds now, privacy exists where bushes once stood open. Dignity is not restored in headlines, but one household at a time.
And with 2030 approaching, Ntaro’s work leaves a final, unavoidable question: if we already know how to end open defecation, if we already have the tools, the evidence, and the people, what, exactly, are we waiting for?

— Makerere University School of Public Health Communications Office, Graduation Profiles Series, 76th Graduation Ceremony
Health
Olivia Nakisita and the Quiet Urgency of Adolescent Refugee Health
Published
7 days agoon
February 18, 2026
Kampala wakes early, but for some girls, the day begins already heavy. In Uganda, nearly three-quarters of the population is under 30, growing up happens fast, and often without protection. One in four Ugandan girls aged 15–19 has already begun childbearing, giving Uganda the highest teenage pregnancy rate in East Africa.
Layered onto this is displacement. The country hosts about 1.7 million refugees, many living in cities like Kampala, where survival depends on navigating systems not designed with them in mind. Also, nationally, 1.4 million people live with HIV, and 70 per cent of new infections among young people occur in adolescent girls, a reminder that vulnerability is rarely singular. When COVID-19 shut the country down, the consequences were immediate, with pregnancies among girls aged 15–19 rising by 25.5 per cent, while pregnancies among girls aged 10–14 surged by 366 per cent.
The numbers tell a story of youth, risk, and quiet urgency. But they do not tell it all. For years, Olivia Nakisita, a public health researcher,has followed how adolescent girls, many of them refugees, navigate pregnancy in Kampala: how far they must travel for care, how early they arrive or delay, and how often services that exist fail to meet them where they are. Her work lives at the uneasy intersection of policy and lived reality, where access does not always translate into care.
February 25th 2026, is the day that her work on whether urban health systems are truly ready for the youngest mothers they now serve will bring her to Freedom Square at Makerere University, where she will graduate with a PhD in Public Health.

Her doctoral journey, focused on maternal health services for adolescent refugees in urban Uganda, has unfolded at the intersection of scholarship, community service, and the daily realities of young girls navigating pregnancy far from home.
The Work That Came Before the Question
Long before she began writing a PhD proposal, Olivia Nakisita was already immersed in adolescent health. As a Research Associate in the Department of Community Health and Behavioral Sciences at Makerere University’s School of Public Health, she taught graduate and undergraduate students, supervised Master’s research, and worked closely with communities. Beyond the university, she led New Life Adolescent and Youth Organization (NAYO), a women-led organisation she founded in 2021 to strengthen access to sexual and reproductive health and rights (SRHR) information and services for adolescents and young people.
It was through this community work that a troubling pattern began to surface.
“During our community service,” she explains, “we noted increasing teenage pregnancies, and we also noted challenges with access to maternal health services by teenage pregnant girls.”

Among those girls were adolescents living as urban refugees in Kampala, young, displaced, often poor, and navigating pregnancy in a city not designed with them in mind.
For Nakisita, the concern deepened through her academic training in Public Health Disaster Management, one such programme that prepares multidisciplinary professionals with the technical expertise and leadership competencies required to plan for, mitigate, respond to, and recover from complex disasters through a public health lens. This programme sharpened Nakisita’s interest in how displaced populations survive within complex urban systems. Uganda’s integrated health model, where refugees and host communities are expected to use the same facilities, appears equitable on paper. In practice, it can be unforgiving.
“I got interested in understanding how these refugees who get pregnant manage to navigate the complexities of integration in host societies like Kampala,” she says. “This was driven by the desire to address their needs and to inform and evaluate existing refugee health policies.”

That desire became the foundation of her PhD.
Asking Hard Questions in a Crowded City
Her doctoral research, “Maternal Health Services for Adolescent Refugees in Urban Settings in Uganda: Access, Utilisation, and Health Facility Readiness,” was conducted in Kampala between November 2023 and August 2024. It combined quantitative surveys with qualitative interviews, engaging 637 adolescent refugees aged 10–19 years, alongside health workers and facility assessments.
Her findings showed high perceived access to maternal health services. Clinics existed. Services were available. Yet utilisation, particularly of antenatal care (ANC), lagged. “About three-quarters of the girls attended at least one antenatal visit,” she explains, “but only about four in ten attended in the first trimester.”
And that gap matters. Public health research shows that early and regular antenatal care allows health workers to detect high-risk pregnancies, initiate supplements such as iron and folic acid, monitor fetal development, and provide psychosocial support. Without it, risks compound silently.
By contrast, her study found that facility-based deliveries were remarkably high, with nearly all adolescent refugees (98.3%) giving birth in health facilities, suggesting that the system was reachable, but uneven.

Where the System Falls Short
Her research went beyond utilisation to examine whether health facilities were actually ready to serve adolescent refugees.
Findings show that lower-level health centres in Kampala were moderately prepared to offer adolescent-friendly maternal health services. Some staff were trained. Some spaces existed. Despite this, critical gaps remained. For instance, facilities lacked essential equipment and supplies. Non-provider staff were often untrained. Separate, private spaces for adolescents were limited. Language barriers complicated care. Overcrowding strained already stretched health workers.
In her qualitative interviews, health workers expressed empathy and willingness to help. Many relied on peer educators and community health workers to reach adolescent refugees. But good intentions were not enough.
“They recommended training of healthcare workers, translators for refugees, and improvement in the availability of essential drugs, supplies, and equipment,” Nakisita notes.
She notes that readiness is not just about infrastructure but about the people, preparation, and priorities.
Research with an Emotional Cost
For Nakisita, working with adolescent refugees required care, not only methodologically, but emotionally.
Finding participants in Kampala was itself a challenge. Unlike settlement settings, urban refugees are dispersed, often invisible. Ethical considerations were constant. Adolescents who had given birth were legally considered emancipated minors, but their vulnerability remained.
Though the thesis focused on systems rather than personal narratives, Nakisita’s earlier work with adolescents informed every decision she made. It shaped how she framed questions, interpreted data, and weighed policy implications. This was not detached research, but careful, deliberate, and grounded.
The Scholar Formed by Continuity
Nakisita’s PhD sits atop more than 18 years of experience in training, research, and community service. She is an alumna of Makerere College School (UCE), 1996 and Greenhill Academy Secondary School (UACE), 1998, a long journey through Uganda’s education system before her Diploma in Project Planning and Management at Makerere University completed in early 2000s.
She would later return eight years later to Makerere University for her Bachelor’s degree in Social Sciences and a Master’s in Public Health Disaster Management, and now a PhD in Public Health.
Her academic rigor is reflected in extensive training across SRHR, impact evaluation, research methods, ethics, disaster resilience, and humanitarian health. She has presented at regional and international conferences and published in peer-reviewed journals on adolescent health, refugee maternal care, gender-based violence, and health systems readiness.
As a PhD student, she supervised three Master’s students to completion, with another currently progressing, quietly extending her influence through mentorship.




When Evidence Demands Action
If policymakers were to act on one lesson from her research, Nakisita says; “Emphasis should be given to maternal health services for adolescents.” “They are high-risk mothers,” she adds.
Her findings call for targeted community-based interventions, outreaches, home visits, and financial support for adolescents who cannot afford prescribed drugs, delivery requirements, or critical tests like ultrasound scans.
They also call for health systems to move beyond one-size-fits-all models, recognising that age, displacement, and poverty intersect to shape how care is accessed and experienced.
Now that her PhD is complete, Nakisita plans to translate research into action. Several papers from her study have already been published. A policy brief is planned to influence decision-making in urban and humanitarian health settings.
When asked what she would say directly to adolescent refugee girls navigating pregnancy in unfamiliar cities, her response is simple and direct.
“If it happens,” she says, “as soon as you find out, go to the nearest health facility and seek care. Always return for the visits as asked by the health worker. Ensure that you deliver in a health facility with a skilled health worker.”

Arrival, Without Illusion
When Dr. Olivia Nakisita steps onto the graduation stage at Freedom Square, applause will follow. But the true significance of that moment lies in health facilities still struggling to adapt; in adolescent refugees whose pregnancies unfold quietly in rented rooms and crowded neighborhoods; in policies waiting to be sharpened by evidence.
Her scholarship does not promise quick fixes but offers clarity.
Among the PhDs conferred at Makerere University’s 76th graduation, her work reminds us that some research does not begin in libraries and does not end with theses. It lives on in the slow, necessary work of making health systems see those they have long overlooked.
— Makerere University School of Public Health Communications Office, Graduation Profiles Series, 76th Graduation Ceremony
Trending
-

 Humanities & Social Sciences2 days ago
Humanities & Social Sciences2 days agoMeet Najjuka Whitney, The Girl Who Missed Law and Found Her Voice
-

 Health6 days ago
Health6 days agoUganda has until 2030 to end Open Defecation as Ntaro’s PhD Examines Kabale’s Progress
-

 Agriculture & Environment5 days ago
Agriculture & Environment5 days agoUganda Martyrs Namugongo Students Turn Organic Waste into Soap in an Innovative School Project on Sustainable Waste Management
-

 General7 days ago
General7 days agoMastercard Foundation Scholars embrace and honour their rich cultural diversity
-

 Health2 weeks ago
Health2 weeks agoCall for Applications: Short Course in Molecular Diagnostics March 2026
