Health
Meet Laura Silovsky, a Makerere University Graduate with Refugee Roots Bridging Continents
Published
1 year agoon

On Tuesday January 14, 2025, under the radiant rays of the Ugandan sun, Laura Silovsky crossed the stage at Makerere University’s 75th Graduation Ceremony to receive her master’s degree in Public Health Disaster Management (MDM). Hers is a story of passion, dedication, and curiosity to rewrite the narrative of global education. Among 1,813 master’s graduates, Laura’s story stood out, as a blend of refugee roots, firefighting bravery, and a drive to decolonize learning.
Laura’s journey began long before her arrival in Kampala. Born in the UK to a father who fled from Czechoslovakia’s dictatorship in the 1970s, she grew up understanding displacement intimately. “My father was a refugee. Why would I fear refugees?” she once asked during her research fieldwork in Uganda’s West Nile, where her empathy bridged divides.
“People in Uganda may not expect that a muzungu could be the child of a refugee, but my family experienced displacement from (what was then) Czechoslovakia as well as the effects of the protracted conflict in Northern Ireland. Fortunate to have been born in the UK, I was raised to appreciate that disasters can affect anyone, anywhere, anytime.
After studying Sustainable Development at the University of Edinburgh, I worked on a behavior change project tackling non-communicable diseases in Scotland,” Laura says.

Her journey twisted through battling Australia’s bushfires and volunteering in a COVID pandemic, but it was Uganda’s welcoming refugee policies and Makerere University’s academic excellence that pulled her in next.
“In 2020, I relocated to Australia, just after the worst bushfires since records began and before the COVID-19 pandemic. The following two years, I qualified as a firefighter and supported bushfire recovery by volunteering with a community-based organization. After gaining some insight into these different disasters, I made the decision to return to higher education, and so I applied for the MDM programme at Makerere in 2022,” says Laura.
Armed with experience in emergency response, Laura was drawn to the field’s multidisciplinary nature and was convinced she needed to expand her expertise beyond immediate recovery efforts. She aimed to explore the full disaster management cycle and the intricate connection between health and environment.
“I needed to combine gaining academic knowledge with developing practical skills, so the field placement offered within the master’s degree in Public Health Disaster Management programme was a major motivator for me,” she shared.
The love for Uganda
Studying at the University of Edinburgh, Laura took a class in Kiswahili, that included a field-based short course on the Tanzanian shores of Lake Victoria. This experience sparked a desire to spend more time in the region, but she knew she needed to expand her skill set in order to genuinely add value to an organisation, if she was on the continent.
“I hoped studying at an East African university would teach me invaluable soft skills needed to work more effectively as an international team member. Makerere University School of Public Health (MakSPH) has a strong reputation, and I wanted to study somewhere that was locally grounded but globally recognized. Uganda’s progressive refugee policies were an added incentive to learn from experts here,” Laura says.
Laura’s intentional choice to decolonize her education
“I came to Uganda to learn from the experts here,” Laura declared, rejecting Eurocentric frameworks. “A big factor for me wanting to study at Makerere University was to decolonize my education, to recognize that the knowledge about responding to public health disasters and supporting refugees is here in Uganda,” she says.
She adds, “When I first arrived, I was quite vocal with my classmates about wanting to challenge that bias and truly acknowledge the wealth of knowledge within institutions like Makerere. The expertise here is invaluable, and I was intentional about decolonizing my education.”

At MakSPH, Laura immersed herself in courses like epidemiology, struggled briefly with statistics, but thrived on critical discussion groups and consultation with lecturers.
Collaborating with classmates from Uganda and across East Africa, she learned Luganda phrases and Somali proverbs, and built a “family” united by late-night study sessions and shared ambitions.
Beyond expectations
For Laura, studying at MakSPH was the best decision she could have made. She is still struck by the faculties’ wealth of academic and professional experience in public health and disaster management.
“I anticipated the programme would focus on applying the knowledge we gain to real-world scenarios. Of course, there were cultural differences that took me time to adjust to. I am grateful to faculty members such as Prof. Christopher Garimoi Orach, for his dedication and support, Prof. Elizeus Rutembemberwa for leading by example and valuing students’ time, and Dr. Justine Bukenya and Dr. Simon Kibira for offering their extensive support as my dissertation supervisors.”
The Fieldwork Attachment that Transformed Laura’s Research Experience
At Rhino Camp refugee settlement in West Nile, Laura’s work took on new meaning. Partnering with the Uganda Red Cross Society, she helped digitize data tools and walked long distances through Tika Zone, inspecting latrines and speaking with South Sudanese girls about their challenges in managing their menstrual health through their project that focused on schools.

“That experience in West Nile influenced my own research ideas, and it was a privilege to later return to Rhino Camp for data collection. I will always remember the long days walking with my research assistants through villages and being graciously welcomed by so many respondents,” she recalls, noting that the experiences crystallized her resolve to advocate for refugee dignity globally.
Life in Kampala
Life in Kampala, with its vibrant energy and unique challenges, was truly a ‘full sensory experience’ for Laura. “My parents live in a small village, so Edinburgh felt like a big city when I moved there. And Edinburgh is much smaller and quieter than Kampala! But on weekends, I loved going downtown to shop at Owino Market or heading to Kyadondo Rugby Club for some pork.”
These spaces were perfect for Laura, offering new cultural experiences, including matooke, a starchy dish not found in the UK, which is mainly eaten in Uganda as a local delicacy and staple meal. Despite the differences in culture, sharing meals with classmates provided Laura with a comforting sense of connection.
Back to academics, navigating the university administrative processes wasn’t seamless initially for Laura, though. She says administrative hurdles such as paper-based systems, could change for the university to comfortably enjoy its strong reputation.
She recalls, right at the beginning, when she couldn’t find sufficient information online to support her to complete her application to join Makerere University. However, she later received support from the University’s International Office that deals with the welfare of international students.
Other university officials, from finance, librarians, program administrators, to academic registrars, played a key role in supporting her in her research and postgraduate training. “The system relies on dedicated individuals,” she noted, calling for digital reforms while praising MakSPH’s “atmosphere of innovation.”
“From my experience, such as when obtaining my transcript, the system relies heavily on individual staff members working around these administrative challenges. I’m grateful for those who helped me navigate this, and I’m interested to see how the university continues its digital transition, as it could greatly streamline processes in the future,” says Laura.
A Bittersweet Graduation Day
On graduation day, Laura’s pride mingled with melancholy. Watching families cheer on graduates, she reflected on classmates sidelined by finances or family crises.
Having gone through the course and interacted with Ugandan students, Laura hints on the common financial and personal challenges preventing many from graduating: family illness, new children, sponsorship falling through.
“I know so many of my classmates had worked so hard and were almost over the finish line but, due to financial challenges or other commitments at home, it wasn’t possible for them to graduate this year,” she says.
“For me, I was able to make the choice to pursue this program before having children, so I had fewer responsibilities at home, and I had also been saving for many years to get the money to pay tuition. Because I knew I had the money for tuition before I started, I could focus on studying. As you know, the reality for many people is that that’s not always possible.
“Small supports can transform student experiences,” Laura emphasized, advocating for systemic empathy. She sees great potential for more pastoral support at the university, citing peers from UCU and Kyambogo who benefited from accommodations like private breastfeeding spaces and flexible deadlines in special circumstances. Such initiatives, alongside financial aid, could significantly improve student welfare.
Still, the ceremony’s electric energy—watched via livestream by her parents in Europe—symbolized hope. “Uganda taught me that collaboration transcends borders,” she reflected.

“You could feel this sense of how hard everyone had worked to reach up to that point and that this was really an opportunity for them to celebrate, particularly by having family and friends around to be able to see. I love the PhD awards, when you see the PhD students coming out and their families rushing up to greet them. To me, that’s the best part of the ceremony, because a PhD requires so much work and commitment, and I think it’s really emotional to see everyone share this moment with their support networks,” she says.
Adding that; “…I was so grateful that the ceremony was streamed online. My family were watching live at home in Europe and it was so special that they could see me on camera and participate in the ceremony that way as well.”
Laura noted striking similarities between Makerere and Edinburgh’s ceremonies, especially the moment when students were asked to turn and thank their families, an emotional and powerful tradition.
Looking Ahead
Now in Tanzania, Laura eyes roles with international NGOs, armed with Ugandan-taught pragmatism and a zeal to challenge Europe’s refugee policies. “MakSPH gifted me more than a degree—it reshaped my worldview,” she says.
“As a muzungu with a Ugandan postgraduate education, I feel privileged to have benefitted from different educational perspectives, and I hope that the skills and knowledge I acquired during my time at Makerere will help me to secure a role with an international NGO. After witnessing the incredible support that Uganda provides to refugees, I also hope to advocate for more dignified policies concerning refugees in Europe,” she shares.
“There’s a spirit of innovation and dedication at Makerere, particularly when passionate lecturers like Prof. Orach, Dr. Roy Mayega, or Dr. Victoria Nankabirwa engaged students through discussion and sharing lived experiences. You could really see a different level of engagement within the students as well. Overall, I’ve had such a fantastic experience at Makerere University.”
“I wouldn’t change a thing,” she smiles.“Except maybe convince more Europeans to study here. Africa’s wisdom is the future.”
You may like
-


Mak 76th Graduation Ceremony: CoNAS Presents 16 PhDs & Best Performing Male Student in the Sciences
-


Medical graduates urged to uphold Ethical values
-


CAES Presents Overall Best Performing Student in the Sciences & a Record 28 PhDs at the 76th Graduation Ceremony
-


Over 9,200 to graduate at Makerere University’s 76th Graduation
-


MakSPH Environmental Health Graduates Trained to Prevent Disease at Its Source
-


Philliph Acaye and the Making of Uganda’s Environmental Health Workforce
Health
MakSPH Environmental Health Graduates Trained to Prevent Disease at Its Source
Published
3 days agoon
February 24, 2026
In most health systems, attention turns to illness after it appears in clinics and hospitals. Environmental Health works earlier, often invisibly, by preventing disease before treatment becomes necessary. At Makerere University School of Public Health (MakSPH), this preventive philosophy shapes the training of students learning to manage health risks at their source, through sanitation systems, safer environments, community engagement, and evidence-based public health action.
This year, as MakSPH presents 29 graduands approved by the Makerere University Senate for the award of the Bachelor of Environmental Health Science (BEHS) degree, four outstanding students graduate with first-class honours. Their journeys, shaped by different personal histories and professional ambitions, provide a clear view of how the School prepares practitioners whose work begins long before patients reach health facilities. Through academic training, field practice, research exposure, and leadership experience, the programme equips graduates to address the environmental and social conditions that determine health outcomes across communities.

Environmental health occupies a distinctive position within public health practice. Rather than focusing primarily on diagnosis or treatment, practitioners work at the intersection of science, policy, and society, addressing risks linked to water and sanitation, food safety, occupational health, climate change, and urbanisation. The discipline demands technical competence alongside communication, systems thinking, and community engagement, capabilities that increasingly define modern public health leadership.
The journeys of Nakulima Bushirah, graduating with a CGPA of 4.58 on February 25, 2026, Mujurani Alphersiiru with 4.44, and Cherop Eric with 4.41, alongside Phillip Acaye, the cohort’s overall best student with a CGPA of 4.63, demonstrate how MakSPH shapes students from varied beginnings into professionals grounded in prevention. Their paths reveal a shared formation that links classroom learning with real-world health challenges and prepares graduates to prevent disease before it occurs.
Bushirah Nakulima’s Turn Toward Prevention

For Bushirah Nakulima, environmental health began during a period of uncertainty. The COVID-19 pandemic repeatedly disrupted her Bachelor of Pharmacy studies at Kampala International University, prompting reflection about the kind of health professional she wanted to become. A conversation with a family friend working in preventive health introduced an alternative path, one focused not on treating illness after onset but on preventing it altogether.
“When I applied to Makerere University in 2022, I was considering two career paths,” she recalled. “I prayed to Allah to guide me toward the best one. When I was admitted to the Bachelor of Environmental Health Science, I accepted it wholeheartedly, and I came to appreciate it even more as I studied.”
Her academic foundation had already demonstrated consistency. She progressed from Melody Junior School in Nansana, where she obtained aggregate eight in 2010, to Shuhada’e Islamic School in Nyamitanga, completing O-Level with 25 aggregates in 2016 and A-Level with 10 points in 2018. Pharmacy initially appeared the logical continuation, yet environmental health offered something broader in scale and impact.
“Environmental Health offered an opportunity to prevent illness and suffering before it occurs,” she explained. “It allows a single intervention, such as WASH or health education, to protect many people at once, and it provides flexibility to work across diverse environments. It offered freedom to operate in various settings, which truly connects with my personality since I love exploration.”
At MakSPH, classroom concepts quickly translated into practice. During her internship at Mukono Municipal Council, she conducted school health education sessions, participated in inspections of markets and abattoirs, and engaged communities facing sanitation challenges. Field exposure deepened her understanding of how environmental conditions directly shape disease patterns, reinforcing prevention as both a scientific and social responsibility.
Leadership further expanded her training. Serving as the 90th Female Guild Representative Councillor (GRC), she represented the School of Public Health in the Student Guild structure, facilitating engagement between students and School leadership on academic and welfare matters. The role strengthened her capacity for representation, negotiation, and collaborative problem-solving, skills central to public health practice, where advocacy and systems engagement are inseparable from technical expertise.
Graduating with a CGPA of 4.58, Bushirah’s research examined roadside vendors’ exposure to air pollution in Kampala, reflecting growing concern about occupational and urban environmental risks. She now plans to pursue advanced training in public health, building on MakSPH’s emphasis on evidence-driven and community-centred practice.
Cherop Eric’s Return to the Classroom

Eric Cherop’s journey into environmental health began not in lecture halls but in community service. Raised in Kapchorwa District, he was shaped by economic hardship and resilience, experiences that informed his commitment to community well-being.
He completed his Primary Leaving Examinations at Chema Primary School, a Universal Primary Education institution, attaining 24 aggregates in 2008. He later joined Sipi Secondary School, where he obtained 37 aggregates at Uganda Certificate of Education in 2012 and continued at the same school for A-Level, earning 8 points at Uganda Advanced Certificate of Education in 2014.
After earning a Diploma in environmental health sciences from Mbale School of Hygiene between 2015 and 2017, he entered public service as an Environmental Health Officer and Community Field Facilitator with Kapchorwa District Local Government. His work included sanitation campaigns, climate resilience initiatives, nutrition education, and household behaviour change programmes. Over time, field experience revealed the limits of practice without deeper theoretical grounding.
“I wanted to understand not only what works in communities, but why it works,” he explains. Enrolling in the BEHS programme at MakSPH in 2022 allowed him to connect practical experience with analytical training. Coursework strengthened competencies in environmental risk assessment, participatory engagement, and data-driven planning. Mentorship reshaped how he interpreted evidence.
“My lecturers helped me move beyond seeing data as numbers,” he said. “I learned to see it as evidence that guides decisions and improves accountability.” Graduating with a CGPA of 4.41, Eric now aims to advance evidence-driven leadership at the intersection of climate change, nutrition, and environmental health, ensuring interventions remain grounded in community realities.
Mujurani Alphersiiru’s Path into Environmental Health

For Mujurani Alphersiiru, Environmental Health arrived at an unexpected moment, when his academic future appeared uncertain. Financial pressures had begun to threaten the continuation of his Bachelor of Nursing Science studies at Kampala International University Western Campus, raising the real possibility that his university education might end prematurely. The turning point came when the government district quota admission list was released, offering him placement at Makerere University under Bunyangabu District and opening an alternative academic pathway he had not previously considered.
At the time, environmental health was unfamiliar to him. “I didn’t know what environmental health was,” he recalls. “But I celebrated because I had reached my dream university.” Orientation sessions and early coursework gradually reframed that uncertainty, revealing a discipline grounded in prevention, systems thinking, and public health policy. What began as an unexpected opportunity soon developed into a clear professional direction.
Serving as class president and 90th Male GRC for the School with Nakulima Bushirah, Mujurani organised student activities, mobilised community outreach initiatives, and advocated for improved learning environments. Balancing leadership responsibilities with academic performance required deliberate discipline and time management.
His educational foundation began at St. Augustine Butiiti Demonstration Primary School in Kyenjojo, where he scored 12 aggregates in 2014. He later attended Pride Secondary School in Mityana, attaining 25 aggregates at O-Level in 2018, before proceeding to Kibiito Secondary School in Bunyangabu, where he obtained 13 points at A-Level in 2021, performance that earned him government sponsorship for university education. At MakSPH, faculty mentorship further strengthened both his academic rigour and commitment to public service.
“Government sponsorship meant responsibility,” Mujurani said. “I had to plan my time carefully while remaining active in school programmes.” Graduating with a CGPA of 4.44, his interests now centre on governance and accountability within health systems, particularly strengthening the implementation of public health policies.
Training Prevention Professionals
Taken together, the three journeys demonstrate how MakSPH’s Environmental Health training converts diverse personal backgrounds into a shared professional orientation centred on prevention. Through interdisciplinary coursework, field placements, research mentorship, and leadership opportunities, students develop competencies that extend beyond technical knowledge to include systems thinking and public engagement.

The BEHS programme, established in 2000 within MakSPH’s Department of Disease Control and Environmental Health, remains the School’s only undergraduate degree and has trained more than 1,000 graduates who now serve across government institutions, non-governmental organisations, academia, and international health programmes. Its continued evolution reflects growing recognition that strengthening health systems requires professionals capable of addressing environmental risks before illness occurs.
The achievements of this year’s graduates, therefore, represent more than academic distinction. They reflect a model of training designed to prepare professionals whose work reduces the need for treatment by preventing disease at its source, reinforcing MakSPH’s role in shaping Uganda’s environmental health workforce.
Health
Philliph Acaye and the Making of Uganda’s Environmental Health Workforce
Published
3 days agoon
February 24, 2026
As Makerere University School of Public Health (MakSPH) presents 29 graduands on February 25, 2026, at Makerere University’s 76th Graduation Ceremony, for the conferment of the Bachelor of Environmental Health Science (BEHS) degree, the journey of the cohort’s best student provides a compelling window into both individual resilience and institutional impact. Philliph Acaye, graduating with a CGPA of 4.63, represents more than academic distinction. His story reflects the lived realities that shape many public health professionals in Uganda and shows how rigorous training can transform experience into leadership within health systems.

Education Shaped by Conflict
Acaye was born on October 2, 1993, in Wangduku Village, Palenga Parish, Pajule Sub-County, Pader District in northern Uganda, a region deeply affected by the Lord’s Resistance Army (LRA) insurgency in the early 2000s, where education and security often existed in constant tension. As a child, schooling unfolded alongside displacement and uncertainty, conditions that shaped an entire generation growing up during the conflict.
“Around 2002, before we had fully moved into the IDP camps, we often ran with our parents whenever there were LRA attacks,” he recalls. “But on several occasions, they caught us unaware. During one of the attacks, they abducted me and moved with me for close to seven kilometres, from Wangduku to Pajule Trading Centre in Pader. At first, they said I was too young to be moved with. I was around nine or ten years old. Later, I understood that someone among them personally knew my father and did not want me taken, so he used my age as the reason, and they left me behind.”

He narrates that several relatives and neighbours, including some of his childhood friends, were not spared, among them an uncle whose whereabouts remain unknown to this day. “If they had gone with me,” Acaye reflects quietly, “I could be dead, or I might not have studied.” The remark sits deep and places his graduation in context, not simply as personal success, but as the outcome of persistence through years when conflict repeatedly disrupted education across northern Uganda.
Between 2002 and 2006, his schooling continued inside Pajule Internally Displaced Persons (IDP) Camp, where families lived in overcrowded settlements and depended largely on relief food. Learning environments were unstable, teachers travelled under risk, and lessons were frequently interrupted by insecurity. Even within the camps, attacks remained possible. Education progressed slowly, but it continued, sustained by families and teachers who insisted that schooling remained essential despite uncertainty.
When communities gradually returned home, Acaye rebuilt his academic track record step by step. He completed Primary Leaving Examinations in 2007 with an aggregate of 19 and was the best pupil at Wangduku Primary School, at a time when enrolment remained low because many families feared returning to villages. He proceeded to Pajule Senior Secondary School, completing O-Level in 2011 with 31 aggregates, and later obtained 10 points at A-Level in 2013 from Kitgum High School.
However, his progression was shaped by consistent recovery after disruption, supported by relatives, teachers, community mentors, and educational assistance from Invisible Children, a post-LRA conflict recovery NGO led locally by Ms. Laker Jolly Okot, which supported his A-Level education.
Professional direction emerged during his training at the Mbale School of Hygiene, where he pursued a Diploma in Environmental Health Science from 2014 to 2016 and graduated with a strong CGPA of 4.4. The diploma opened immediate employment opportunities in community and humanitarian health settings back home, followed by service in local government. Today, he works as a Health Inspector in Kitgum District Local Government, implementing sanitation monitoring, infection prevention activities, and community health interventions. Practical experience strengthened his understanding of public health challenges but also revealed limits in technical depth that he felt required further training.
Training the Public Health Professional
His admission to MakSPH in 2022 through the government diploma-entry sponsorship scheme represented a deliberate academic decision rather than a career reset. He sought broader analytical skills and a stronger grounding in environmental health systems, particularly in areas of surveillance, planning, and evidence-based decision-making.
“I realised some technical aspects were not fully covered at the diploma level. I wanted to understand public health beyond implementation and learn how decisions are justified scientifically,” Acaye explained.

The sponsorship, he observed, transformed that ambition into possibility and remains central to how he understands his academic journey at Makerere University. “I am grateful to the Makerere University selection committee, the MakSPH selection committee, and the Government of Uganda for this opportunity. Opportunities like this are not guaranteed, and I recognise the trust placed in me to undertake and complete the three-year BEHS programme.”
The transition into university study was not seamless, though. His admission had come earlier than planned, and he began coursework without formal study leave while still tied to workplace obligations in Kitgum. Sustained support from district leadership, particularly Dr. Okello Henry Otto, the District Health Officer, eventually enabled him to secure study leave and concentrate fully on academic work. Now with stability came rapid academic improvement, supported by peer learning, faculty mentorship, and a strong curriculum that emphasised analytical reasoning alongside applied practice.
Acaye attributes his transformation to the programme’s academic culture rather than individual brilliance. “The programme helped me realise that what I was doing before was only a surface understanding,” he argued. “I learned to approach public health more deeply.” Exposure to research methods, he revealed, reshaped how he interpreted field experience and encouraged him to submit an abstract to an international academic conference, marking his transition from practitioner to emerging researcher.
For Mr. Abdallah Ali Halage, the MakSPH Coordinator of the BEHS programme, such outcomes reflect intentional design rather than coincidence. He noted that student success is rooted in a training philosophy that combines technical instruction with professional discipline from the moment students enter the programme. According to him, orientation focuses not only on coursework but also on expectations of conduct, independence, and responsibility. “When students join, we brief them on how seriously they must approach their academic journey,” he said. “That grounding helps shape their performance over time.”

Mr. Halage argued that while some high-performing students enter through diploma schemes, achievement ultimately depends on commitment and effort rather than background. He cited Acaye’s consistent curiosity and self-motivation as defining traits, noting that strong academic results tend to follow students who actively engage with the learning process.
“I congratulate Philliph and his colleagues upon attaining first-class honours and performing very well academically. Philliph has been hardworking and self-motivated. He has consistently shown a strong interest in his studies, and that commitment has helped him achieve this result. He has been a very good student,” Mr. Halage attested.
He added that the achievement reflects a broader culture within the programme. “Our students are disciplined and independent. Their commitment, together with support from the School management, the College and University leadership, has contributed greatly to their success.”

From Individual Achievement to Institutional Impact
The broader significance of Acaye’s achievement becomes clearer when placed within the evolution of the BEHS programme itself. Established in 2000 within MakSPH’s Department of Disease Control and Environmental Health (DCEH), the programme remains the School’s sole undergraduate degree and was among the earliest environmental health bachelor’s programmes in East Africa. In more than two decades, it has produced over 1,000 graduates, expanding professional capacity beyond diploma-level training and strengthening Uganda and the region’s environmental health workforce across government, non-governmental organisations, educational institutions, and points of entry such as airports and border services.
Mr. Halage explained that the programme helped redefine career pathways within the government of Uganda’s public service structures by introducing degree-level expertise into environmental health roles. Graduates now serve as Environmental Health Officers, Senior Environmental Health Officers, and technical specialists contributing to policy implementation and service delivery across multiple sectors. The academic pathway has also expanded vertically, with postgraduate training opportunities at MakSPH currently enabling graduates to progress into research, teaching, and doctoral-level specialisation, ensuring continuity within the discipline.

A Programme Shaping Regional Practice
The reputation of Makerere University’s Bachelor of Environmental Health Science programme is also increasingly influencing regional institutions. During a strategic benchmarking visit to MakSPH on July 30, 2025, Dr. Ratib Dricile, Dean of the Faculty of Health Sciences at Muni University, described the School of Public Health as a reference point for universities seeking to strengthen environmental health training in the region.
The main reason the delegation visited Makerere University School of Public Health was that Muni University remains a young and growing institution located in north-western Uganda along the borders with the Democratic Republic of Congo and South Sudan, where porous borders contribute to frequent cross-border diseases, many of which are preventable through strong environmental health approaches, Dr. Dricile explained.

“Makerere University, with over 100 years of institutional experience and 25 years running the Environmental Health programme, was the right place for us to benchmark, particularly in curriculum design, course content, programme structure, and implementation,” he said. “We were impressed by the work being implemented and gained more than we initially expected. By integrating these experiences, we believe the Muni University curriculum can become even stronger. The collaboration will allow us to adopt innovations built on Makerere’s long experience, and we believe that working together with Makerere University will strengthen Muni University institutionally and contribute positively to our university’s growth and ranking.”
It is within this institutional tradition, built over decades of training environmental health professionals across Uganda and the region, that Philliph Acaye’s achievement takes meaning. For him, graduating top of the class remains grounded in practical purpose rather than prestige. He views a first-class degree as an opportunity rather than an endpoint. Recalling guidance from his lecturers, he said strong academic results can open doors but must be followed by demonstrated competence. “A first class helps you get shortlisted,” he said. “After that, you must prove yourself.”

His immediate plans reflect that perspective. He is currently pursuing additional training in Health Services Management at Gulu College of Health Sciences while preparing for postgraduate study in either public health or environmental and occupational health. At the same time, he continues supporting pupils in his community and plans to mobilise resources to provide sanitary pads for girls at his former primary school, an initiative he believes will help reduce school dropout rates in rural areas.
Acaye’s journey, from disrupted schooling in an IDP camp to graduating top of MakSPH’s BEHS programme for the 2022 cohort, reflects the deeper purpose of public health education. As MakSPH presents its newest cohort for graduation this week, his story demonstrates how the programme turns lived experience into professional capacity, strengthening communities and health systems across Uganda and the region, one graduate at a time.
Health
Makerere University School of Public Health Graduates First Cohort of Cost-Effectiveness Analysis Short Course
Published
7 days agoon
February 20, 2026By
Mak Editor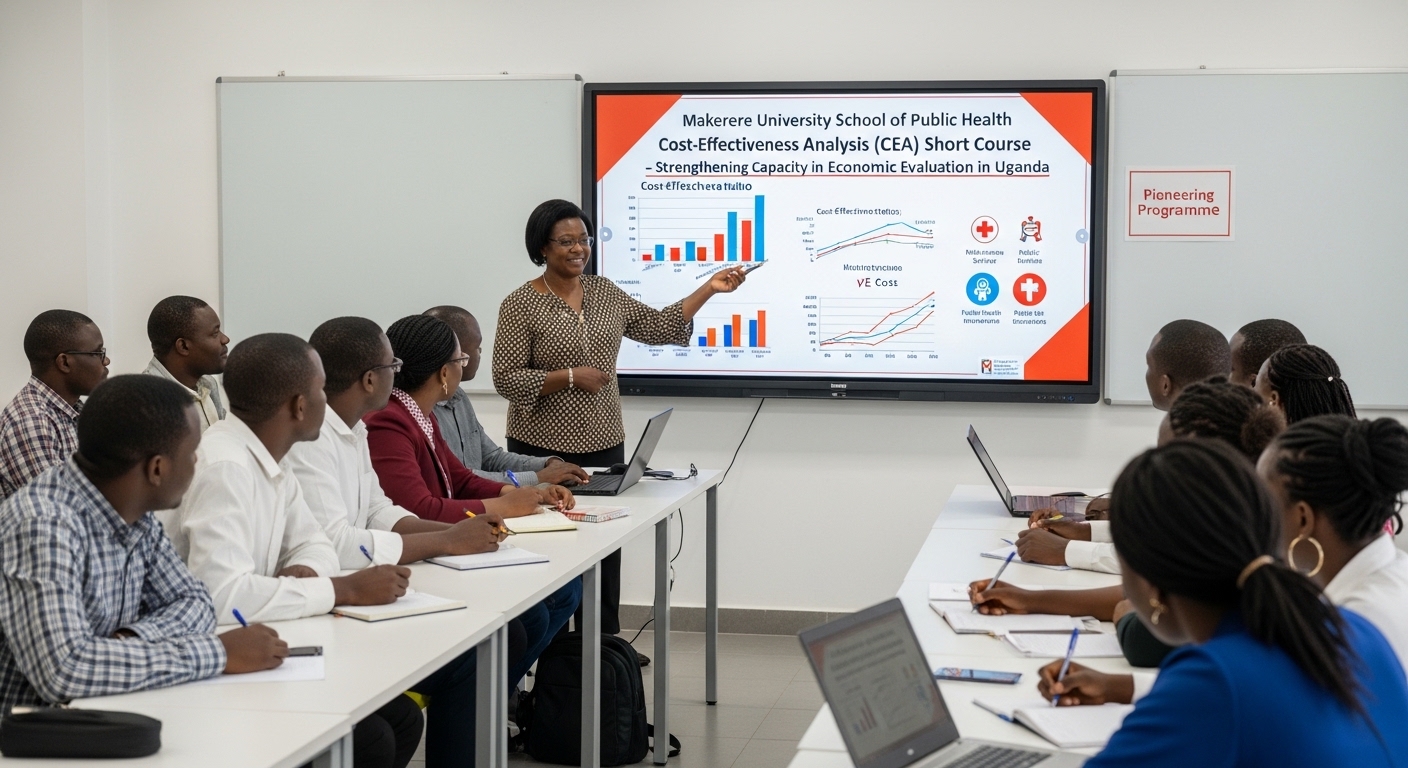
Kampala, Uganda – The Makerere University School of Public Health (MakSPH) has marked a significant milestone with the graduation of the first-ever cohort of its Cost-Effectiveness Analysis (CEA) Short Course. The pioneering programme is designed to strengthen capacity in economic evaluation in Uganda and beyond.
The virtual graduation ceremony honored eleven (11) participants who completed the course. The cohort included professionals from academia, research institutions, government agencies, and non-state actors, reflecting the increasing demand for skills in economic evaluation across sectors.
The short course was developed and implemented by the Department of Health Policy, Planning, and Management (HPPM) in response to the increasing need for evidence-informed decision-making in a context of limited resources.
In her remarks during the ceremony, Assoc. Prof. Suzanne Kiwanuka, Head of the Department of Health Policy, Planning and Management (HPPM) at MakSPH, congratulated the inaugural cohort for completing what she described as a “critical and timely” course.
“With decreasing resources and rising demand for services driven by population growth and the emergence of high-cost technologies, decision-makers must make difficult choices,” she noted. “Cost-effectiveness analysis is no longer optional. It is central to conversations in the corridors of power.”
The CEA short course was designed to equip policymakers, researchers, and practitioners with both theoretical knowledge and practical skills in economic evaluation. Participants were introduced to key principles of health economics, costing methodologies, decision-analytic modelling, Markov modelling, sensitivity analysis, and interpretation of incremental cost-effectiveness ratios (ICERs).
According to Prof. Elizabeth Ekirapa, the course lead at MakSPH, this inaugural offering had been “a long time coming,” following years of discussions within the department about building local expertise in economic evaluation.
Delivered over 10 days through interactive online sessions, the course combined lectures, case studies, and hands-on modelling exercises using contextually relevant datasets. Participants were required to develop and present applied cost-effectiveness projects as part of their assessment, allowing them to translate theory into practice.
During the feedback session at the graduation ceremony, faculty emphasized the importance of clarity in defining study perspectives, selecting appropriate outcomes, and aligning research questions with modelling approaches.
Dr. Chrispus Mayora, one of the facilitators, highlighted the need to carefully select outcomes that directly reflect the intervention being evaluated. “When thinking about outcomes, ask yourself: Is this aligned with what I want to study? Interesting outcomes are not always the most appropriate ones,” he advised.
Participants were also encouraged to select modelling techniques such as decision trees or Markov models based on the research question and the nature of the disease or intervention under study.
Prof. Ekirapa described the graduates as “trailblazers,” noting that their feedback would shape future iterations of the course. “When you are the first cohort, you are like pioneers,” she remarked. “We are committed to improving this course to ensure it becomes a world-class programme.”
For many attendees, the graduation ceremony was a new experience, as certificates were awarded virtually an approach that participants welcomed as innovative and inclusive.
“Cost-effectiveness analysis enables us to maximise value for money,” noted Dr. Crispus Mayora of MakSPH. “It allows decision-makers to compare interventions systematically and ensure that limited resources achieve the greatest possible benefit.”
The programme aligns with Makerere University’s broader mandate to provide high-quality training that responds to national and regional development priorities. Participants who successfully complete the course receive a certificate signed by the Dean of the School of Public Health.
As the ceremony concluded, faculty encouraged continued engagement beyond the classroom. Graduates were urged to refine their project ideas and collaborate with the department in advancing research and policy discussions.
The successful completion of the first CEA short course marks an important step in building a cadre of professionals equipped to conduct rigorous economic evaluations. With plans to expand and refine the programme based on participant feedback, the HPPM department under MakSPH is positioning itself as a regional leader in health economics and policy analysis training.
Trending
-

 Humanities & Social Sciences4 days ago
Humanities & Social Sciences4 days agoMeet Najjuka Whitney, The Girl Who Missed Law and Found Her Voice
-

 Health1 week ago
Health1 week agoUganda has until 2030 to end Open Defecation as Ntaro’s PhD Examines Kabale’s Progress
-

 Agriculture & Environment7 days ago
Agriculture & Environment7 days agoUganda Martyrs Namugongo Students Turn Organic Waste into Soap in an Innovative School Project on Sustainable Waste Management
-

 General1 week ago
General1 week agoMastercard Foundation Scholars embrace and honour their rich cultural diversity
-

 General3 days ago
General3 days ago76th Graduation Highlights
