Health
Study Reveals Epilepsy Prevalence & Treatment Barriers in Uganda, Urgent Need for Awareness & Resources
Published
2 years agoon
By
Mak Editor
By Davidson Ndyabahika & Julius Mugaga Tukacungurwa
A new study conducted in Uganda has unveiled the prevalence of epilepsy and identified significant barriers to treatment. The study conducted by Makerere University School of Public Health in partnership with Ministry of Health and Duke Global Neurosurgery and neurology, utilized community-based screening methods, found that urgent action is needed to increase awareness and allocate more resources to address this pressing public health issue.
Nearly 80% of individuals with epilepsy reside in low- and middle-income countries (LMICs), and a staggering 75% of those with epilepsy in LMICs do not have access to treatment. This alarming trend is further exacerbated by the stigma surrounding epilepsy, which often leads people to avoid seeking medical care due to fear of discrimination or social ostracization. The study underscores the urgent need to address the barriers to treatment, including stigma, and allocate more resources to improve epilepsy care in LMICs.
By providing a community-based descriptive statement about epilepsy in Uganda, this study sought to contribute vital information for intervention planning, addressing the urgent need for increased awareness, support, and access to treatment for people living with epilepsy in Uganda.
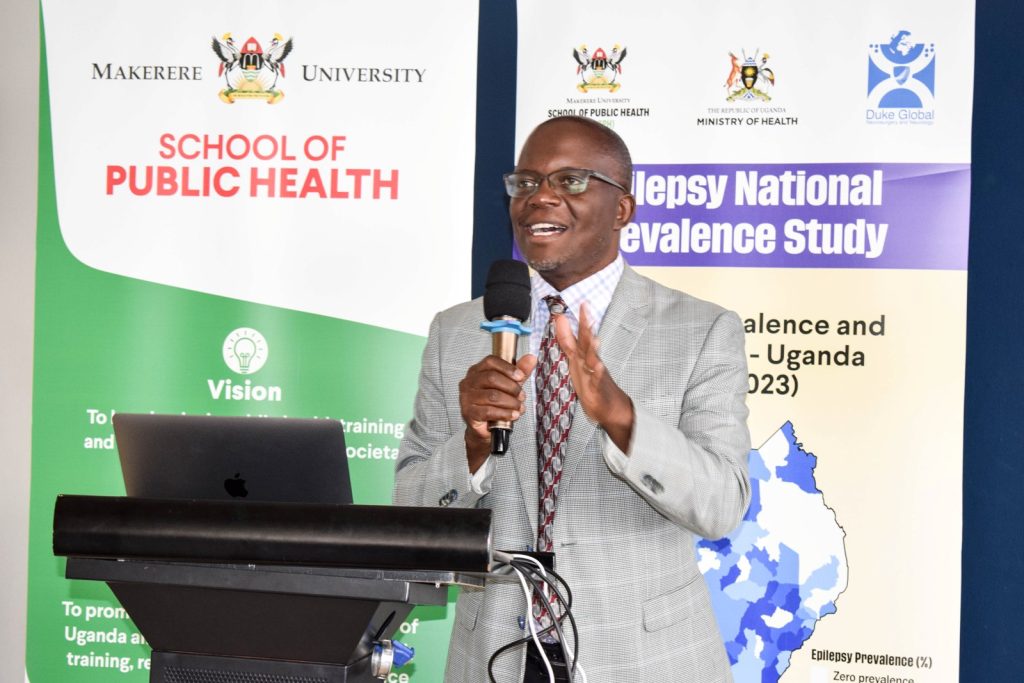
At the Epilepsy National Prevalence Study Dissemination and Dialogue meeting held on Wednesday, April 5, 2023 at the Golden Tulip Hotel in Kampala, Professor Anthony Fuller, the USA & Duke Neurosurgery Principal Investigator, revealed concerning findings.
The study unveiled that the national prevalence rate of epilepsy in Uganda is alarmingly high at 1.69 per cent, indicating that over 770,000 Ugandans are living with the disease. Professor Fuller’s presentation shed light on the urgent need for increased awareness, support, and intervention for those affected by epilepsy in Uganda.
During the investigation, participants were asked about their experiences with epilepsy, including symptoms such as shaking, falling, loss of consciousness, bladder control, and abnormal sensations. These questions were part of the primary screen in Phase One of the study, aimed at gathering information on epilepsy-related experiences in the past year.
With a meticulous screening process, the study examined 35,056 individuals suspected to have epilepsy, of whom 2,284 were found positive for unadjusted epilepsy, translating to a prevalence rate of 6.52% in the primary phase.
In the secondary phase, 732 individuals were confirmed positive for unadjusted epilepsy, resulting in a prevalence rate of 2.09%. In this phase, participants were asked about the frequency of attacks, occurrence in children during fever, and association with malaria-related hospitalization. These questions sought to gather additional information to aid in assessing and analyzing the nature and context of participants’ experiences with epilepsy.
Through rigorous clinical validation, including Neuro validation and electroencephalogram (EEG) tests, 594 individuals were confirmed to have epilepsy, bringing the final prevalence rate to 1.69%.
In the Central region, out of 11,746 individuals screened, 198 were confirmed positive for epilepsy, while 11,548 were negative, resulting in a prevalence rate of 1.69%. In the Eastern region, 125 out of 5,776 screened were positive, with a prevalence rate of 2.16%. In the Northern region, 68 out of 5,037 screened were positive, resulting in a prevalence rate of 1.35%. Lastly, in the Western region, 203 out of 12,497 screened were positive, with a prevalence rate of 1.62%.
These regional findings shed light on the distribution of epilepsy cases in Uganda and highlight the need for tailored interventions and support at a local level. “The epilepsy prevalence is unevenly distributed, ranging from zero to over 5% in specific districts,” says study report.
Dr. Fredrick E Makumbi, an Associate Professor and a Ugandan Principal Investigator for the study from MakSPH, highlighted the gap in community awareness regarding epilepsy treatment, leading to an increased prevalence rate.
He pointed out that the youth, aged 18 to 35, had a prevalence rate of 2.37 percent, while those aged 36 to 60 had a prevalence rate of 2.33 percent. Along with other investigators and participants, Professor Makumbi emphasized the need for further studies to identify driving factors and take equitable action.
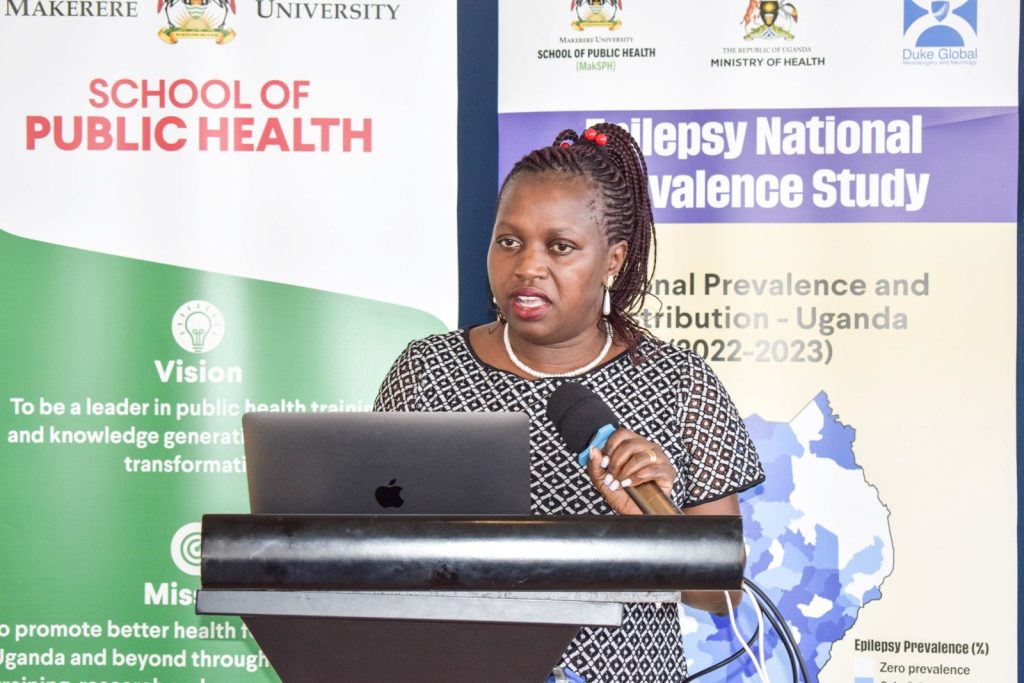
Dr. Angelina Kakooza Mwesige, a Co-Principal Investigator for Uganda who is also a Senior Lecturer and Paediatric Neurologist in the Department of Paediatrics and Child Health, Makerere University School of Medicine noted interesting gender regional variations of epilepsy with higher prevalence in women compared to men.
In the Eastern region, the prevalence rate was higher in females at 2.40% compared to males at 1.97%. Similarly, in the Central region, the prevalence rate was 1.81% in females and 1.53% in males. In the Northern region, the prevalence rate was 1.33% in females compared to 1.37% in males, while in the Western region, it was 1.54% in females and 1.72% in males.

This revelation according to Dr. Kakooza has prompted further consideration for conducting a specialized study to investigate the underlying factors contributing to this statistic.
“We found the overall prevalence rate is 1.73% in female compared to 1.63% in male. We do not know the reason yet but we are investigating this. Also, what we found out, the medicine that can help treat this disease and the trained specialists are not enough. We need to ensure equal and free access to medicine for all. I appeal to all Ugandans, a person with this disease, just like any other disease deserves our support and care,” said Dr. Kakooza.
Dr. Daniel Kyabayinze, the Director of Public Health at the Ministry of Health -Uganda, thanked the researchers for the great study and acknowledged that epilepsy requires lifelong treatment and highlighted the need to continuously provide treatment for all those affected.
According to Dr. Kyabayinze, the government plans to use the study’s findings to estimate the treatment needs, and Kyabayinze expressed confidence that further examination by Makerere University School of Public Health’s partners will help identify associated factors, such as potential agents or organisms, that can be modified to combat epilepsy. He also noted that while some individuals are already receiving treatment, many Ugandans face challenges in affording the necessary treatment for epilepsy.
Dr. Kyabayinze emphasized the importance of placing mental health specialists in various locations across the country to ensure access to services, stating, “There is also a need to intensify sensitization efforts to avoid stigmatizing people with epilepsy and ensure they receive the services they need.”

Ms. Nina Mago, Founder and Program Advisor of Purple Bench Initiative, underscores the need policy makers to prioritize healthcare needs of individuals with epilepsy to needs of people with epilepsy. She emphasizes affordable access to good quality medication.
“When you have medication, you have less seizures and you become more confident on being independent, to participate in activities which may include going to school, holding up a job, social interaction but all this is possible when there is also strong awareness,” says Nina.
Ms. Mago, says epilepsy is a life-threatening condition; “I came up with a connotation of a phone battery, as a notification of battery low shows up, equally relates to a life about to be lost.”
Dr. Olaro Charles, the Director Health services – Clinical in the Ministry of Health stated that epilepsy remains one of the common mental health conditions in Uganda. He said that they have just concluded a joint review mission and found out that from all their mental health facilities, epilepsy constitute to almost 55.4% of patients.
“If you look at 2019/2020 they were about 314,000 then came to about 340,000 and then last year it was 251,000. This mapping however is very important because it helps us to plan for care. If we do the same in those regions with high prevalence, we may be able to plan well”. Dr. Oralo.
Dr. Sarah Nekesa, Executive Director of Epilepsy Support Association Uganda, called on members of Parliament to increase the budget for mental health drugs, including epilepsy medication, and ensure their availability. She emphasized the need for integrating epilepsy services with other healthcare services to improve accessibility.
Additionally, Dr. Nekesa highlighted the importance of grassroots awareness to combat stigma, and urged the government to allocate adequate human resources and support from health workers to encourage peer talks and build confidence among people living with epilepsy.
“We should increase the drug availability in health facilities and make sure that a person with epilepsy is able to get medication whenever they need it. Epilepsy is not understood by everyone so if everybody understands epilepsy it would be easier for treatment and stigma to go down and integration of epilepsy in every service that is given to the community”. Said Dr. Nekesa.

You may like
-

Simplicity, Service & Scholarship: Hallmarks of Professor Livingstone Luboobi’s Legacy
-


EfD-Mak Holds 2nd Advisory Board Meeting: Charts Path for Growth
-


Public University Legal and Accounting Officers Trained on Governance and Compliance
-


Celebrating the Life of Prof. Livingstone Sserwadda Luboobi
-

Fare Thee Well Prof. Luboobi
-


Strengthening Grants Management Through Institutional Collaboration and Capacity Building
General
Strengthening Grants Management Through Institutional Collaboration and Capacity Building
Published
4 days agoon
July 15, 2025
As the funding to the higher education sector keeps on reducing due to competing priorities, universities are implored to come up with structures and strategies to attract and win research grants.
Key findings indicate that universities with institutionalized grant management offices, strong and coordinated research teams are better positioned to effectively compete for grants.
Makerere University, in partnership with Northwestern University, is spearheading the E-SMAC G11 Grants Administration and Management workshop from 14th to 17th July 2025, aimed at strengthening grant management offices and systems among the participating universities and entities.
It is envisioned that through this capacity building approach, the workshop which brings onboard over 130 participants from different universities and entities, will address the knowledge and skills gaps among faculty, grant managers, administrators and support staff.
The participating universities and entities include: Makerere University, Uganda Christian University-Mukono, Soroti University, Gulu University, Clarke International University, King Ceasor University, Kyambogo University, Muni University, Mother Kevin University, Uganda Martyrs’ University-Nkozi, Ernest Cook University, Mbarara University of Science and Technology, University of Kisubi, Kabale University, Busitema University, BRAC University, Infectious Diseases Institute, Ministry of Health, and among others.
Makerere University and Northwestern University have built a strong partnership over the past decade through academic exchange, collaborative research, and capacity building initiatives. “Since 2020, the institutions have deepened their collaboration in research administration through the UASP fellowship, sharing best practices and co-developing of sustainable systems to strengthen research management,” said Prof. Sylvia Antonia Nakimera Nannyonga-Tamusuza, Head of Grants Administration and Management Support Unit (GAMSU) at Makerere University.
She informed the participants that Northwestern University has been instrumental in building the capacity of staff at Makerere University in grants writing, management and administration.

Prof. Nannyonga-Tamusuza testified that when she was appointed to head GAMSU, she received comprehensive training from Northwestern University, which enhanced her competences and expertise in the field. She acknowledged Kate Klein from Northwestern University for the mentorship that empowered her with valuable knowledge and skills. She reported that five (5) members of staff from Makerere University had been trained by Northwestern University in grants and research management.
Filled with joy, she introduced the team of experts from Northwestern University namely Kate Klein, Bethany Ekesa and Elizabeth Christian to Makerere University, and applauded them for accepting to be facilitators. Prof. Nannyonga-Tamusuza assured the workshop participants that the team from Northwestern University would not only train them, but would share best practices in grants management and administration as well as networking opportunities.
The training workshop is part of the Expanded Strengthening of Makerere University’s Research Administration Capacity (E-SMAC) program, which focuses on enhancing research administrative systems and staff capacity at Makerere University and its partner institutions. Mordecai Tayebwa is the Program Director and Principal Investigator of the E-SMAC program being implemented from July 2024 to December 2025. The program is funded by the National Institute of Allergy and Infectious Diseases (NIAID).
The workshop provides a platform to build faculty, grant managers and administrators capacity in grant writing and management, foster cross-functional collaboration across departments, strengthen understanding of budget creation, biosketch and funder systems, encourage mentorship and peer to peer learning, and lay a foundation for regular support.
The training tackles four broader themes namely Grants Introduction and Systems, Proposal Development, Capacity Building, and Outcomes and Forward Planning. It covers vital areas such as grant writing, budgeting, funder systems, compliance, and overall grant administration. It features practical sessions, mentorship opportunities, and collaborative learning, with the goal of strengthening pre-award and post-award grant management and improving research productivity and compliance.

Opening the workshop, the Acting Deputy Vice Chancellor (Finance and Administration) at Makerere University, Prof. Winston Tumps Ireeta urged universities to institutionalize grant management offices and policies as well as strengthening research systems through collaborations.
Sharing his experience, Prof. Ireeta informed the participants that he was involved in the strategic discussion that led to the establishment of GAMSU at Makerere University. “We observed that Makerere University School of Public Health had established a grants office, which was instrumental in attracting and winning funds for research. We were inspired by this best practice. Thus, a comprehensive policy was developed to streamline and strengthen grants management across all colleges at the University,” he said.
Prof. Ireeta noted that Makerere University commits to being a research-driven institution, a strategic direction, that needs a strong funding base. ‘Research grants are therefore a key resource,” he said.
Stressing the importance of adhering to the technical details in the grants management processes, Prof. Ireeta appealed to the participants to be active listeners and maximally utilize the moment to learn from the experienced facilitators.

In the same vein, Prof. Nannyonga-Tamusuza, applauded the University Council and Management for the strategic direction undertaken to elevate GAMSU from a Unit to a Directorate. This points to the central role of the grants office in the life cycle of Makerere University. She pointed out that GAMSU reports to the Vice Chancellor through the Deputy Vice Chancellor (Finance and Administration).
Established by the University Council in 2020, GAMSU is a central office at Makerere University. It provides professional and coordinated services across the entire grant life-cycle-from identifying funding and developing proposals to ensuring compliance, project execution, financial oversight, and institutional capacity building. GAMSU works closely with academic and administrative staff to support competitive, well-managed and accountable research.
Focusing on the training workshop, Prof. Nannyonga-Tamusuza called upon the participants to utilize the golden opportunity to deepen their understanding of grants management in advancing research. She acknowledged the role of this collaboration in fostering mutual learning and the sharing of best practices, noting that such initiatives were key in ensuring that research conducted by universities aligns with global standards. She encouraged participants to engage fully in the workshop, collaborate with their peers, and build lasting connections to foster continuous learning.
The Administrative Director of the Havey Institute for Global Health at Northwestern University, Kate Klein, noted that grants administration goes beyond securing funding. She explained that grant administration is about building strong, sustainable systems that support researchers, facilitate collaboration, and ultimately contribute to solving global challenges.
Klein stated that grants administration and management require continuous learning, adaptability, and a strong foundation in regulatory and financial oversight.
“Collaborating and learning from one another is essential,” Klein stated. “When grants administration is effectively managed, it becomes a powerful catalyst for driving impactful change in research, ultimately advancing global initiatives that address the world’s most pressing challenges.”

She urged participants to critically analyze their current systems and identify areas where improvements could be made. By doing so, they would be better positioned to manage grants effectively and maximize their impact. She guided that a research grants administrator should be able to design monitoring frameworks, liaising with funders to address grant-specific issues, coordinating compliance, budgeting and reporting to ensure timely and effective implementation.
Presenting the Existing Support Systems and Principal Investigator (PI) agreements, Prof. Nannyonga-Tamusuza pointed out the critical role of GAMSU in maximizing Makerere University’s access to grants. This is particularly important in the context of limited financial resources, where GAMSU ensures that the university effectively leverages available funding opportunities.
Prof. Nannyonga-Tamusuza explained that GAMSU ensures research projects align with the priorities of funders and comply with both institutional and external regulations. She emphasized that this alignment is essential for securing and managing grants successfully. She stated that oversight offered by GAMSU, helps streamline the process for researchers. She pointed out that grant management is a collaborative process, involving multiple stakeholders across the university, which ensures that the necessary expertise and support are in place to manage grants effectively.
Underscoring the importance of grant negotiations, particularly with sub-award grants, Prof. Nannyonga-Tamusuza clarified that such negotiations are most successful when managed at the institutional level, where GAMSU oversees the entire lifecycle of a grant-from identifying funding opportunities to post-award activities.
Harriet Nambooze, the Project Coordinator at Makerere University School of Health Sciences, provided participants with a detailed guide on navigating the National Institutes of Health (NIH) grant application process. She introduced essential tools such as Grants.gov, eRA Commons, SAM.gov and the NATO Commercial and Government Entity (NCAGE), which are critical for applying and receiving an NIH award.

Nambooze stressed the importance of accurately setting up roles in the eRA Commons system, including Signing Official (SO), Principal Investigator (PI), Account Administrator (AA), and Administrative Official (AO), as well as ensuring that profiles are up-to-date across various systems.
She highlighted the necessity of adhering to NIH’s strict submission deadlines and maintaining active individual and institutional profiles to facilitate timely applications. She recommended that institutions should appoint multiple Signing Officials (SOs), to avoid any delays with the required submissions.
Presenting to the participants, Mordecai Tayebwa shared a detailed, step-by-step guide to starting a new grant application. He explained the key elements of the grant process, including the necessity of including a budget, adhering to specific formatting guidelines, and uploading required documents, such as the foreign justification for international projects.

He pointed out the need of thoroughly verifying the application before submission to ascertain that all required documents are included. “This step is crucial to avoid errors that could delay or jeopardize the submission,” he said.
The first day of the workshop set a strong foundation for enhancing grant administration capacity among the participating universities. Participants were equipped with knowledge and skills in grant systems at the national and global levels.
Day two, will focus on topics such as reading funding opportunity announcements, tailoring writing, budget development and justification, sub-contract management, sub-recipient monitoring, and Memoranda of Understanding (MoUs).
On Day three, the participants will gain a deeper understanding of the Grants Office, financial management, internal controls and reporting, peer review process overview and project closeout.
On Day four, the participants will witness the launch of the MakGAP (Makerere University Grants Professional Initiative), listen to a keynote speech on grants management from the Vice Chancellor of Makerere University, Prof. Barnabas Nawangwe, as well as presentations on professional growth through MakGAP, CRA Exam, and Global Research Administration Networks, and professional recognition of research managers and administrators in Africa and post evaluation.
The first day of the workshop set a strong foundation for enhancing grant administration capacity among the participating universities. Participants were equipped with knowledge and skills in grant systems at the national and global levels.
Day two, will focus on topics such as reading funding opportunity announcements, tailoring writing, budget development and justification, sub-contract management, sub-recipient monitoring, and Memoranda of Understanding (MoUs).
On Day three, the participants will gain a deeper understanding of the Grants Office, financial management, internal controls and reporting, peer review process overview and project closeout.
On Day four, the participants will witness the launch of the MakGAP (Makerere University Grants Professional Initiative), listen to a keynote speech on grants management from the Vice Chancellor of Makerere University, Prof. Barnabas Nawangwe, as well as presentations on professional growth through MakGAP, CRA Exam, and Global Research Administration Networks, and professional recognition of research managers and administrators in Africa and post evaluation.
Health
Ugandan Study Flags Girls and Senior Students as a Mental Health High-Risk Group
Published
7 days agoon
July 12, 2025
Based on research led by Max Bobholz and colleagues from Makerere University in Uganda, Essentia Institute of Rural Health, and the Medical College of Wisconsin in the United States.
Adolescence is meant to be a time of holistic growth and self-discovery, but for many Ugandan teenagers, this period is becoming a season of silent mental health struggles. A new study published in PLOS Global Public Health has uncovered a silent but growing crisis: nearly one in five Ugandan secondary school students in the study areas have signs of an emotional disorder. These conditions included anxiety, depression, post-traumatic stress disorder (PTSD), and adjustment disorders often involving excessive worry, sadness, fear, or mood instability. Also, one in 20 adolescents exhibited behavioral issues ranging from attention-deficit/hyperactivity disorder (ADHD) and oppositional defiant disorder to substance use and other risky behaviors like alcohol use.
The study, led by Max Bobholz, a PhD candidate in Public and Community Health at the Medical College of Wisconsin, surveyed a sample of 1,953 students aged 10 to 18 years enrolled in eight secondary schools in Iganga district in Eastern Uganda and Mukono district in Central Uganda. This was one of the most comprehensive efforts yet to understand the prevalence and drivers of mental health challenges among school-going Ugandan adolescents.
“We are looking at a generation facing a complex blend of stressors, namely, academic, social, and emotional,” says Bobholz. “Our findings show that certain groups are especially vulnerable, and schools need to be equipped to respond.”
This study results, published on June 12, 2025 was funded by the Swedish International Development Cooperation Agency (SIDA), a government agency of the Swedish Ministry for Foreign Affairs, through the Makerere University Postdoctoral Fellowship to one of the investigators, Dr. Catherine Abbo. Other researchers included Julia Dickson-Gomez, Arthur Kiconco, Abdul R. Shour, Simon Kasasa, Laura D. Cassidy, and Ronald Anguzu.
According to the study, girls bear a higher emotional burden. Researchers found that female students had nearly two times higher odds of suffering from emotional disorders such as anxiety or depression than their male peers.
Dr. Catherine Abbo, an Adolescent Psychiatrist and Associate Professor at Makerere University, attributes this to both biological and socio-cultural factors. “Puberty brings hormonal shifts that can heighten emotional sensitivity,” she explains. “But just as importantly, Ugandan girls often face intense pressure to conform to gender roles while also navigating issues like body image, harassment, and future uncertainty.” The researchers are calling for gender-sensitive mental health interventions, particularly in schools, where early support could help mitigate long-term mental health issues.

Higher associations in older teens?
Age also emerged as a key associated factor, with each additional year increasing the odds of behavioral disorders by 20%. “As adolescents grow older, they are more prone to risk-taking, impulsivity, and resistance to authority,” explains Dr. Simon Kasasa, a senior lecturer and biostatistician at Makerere University School of Public Health.

“Combine that with academic pressure and identity-related stress, and it’s no surprise we’re seeing more conduct issues in late adolescence,” Dr. Ronald Anguzu, an Assistant Professor in the Institute for Health and Humanity at the Medical College of Wisconsin, added. This study raises critical questions about whether and how Ugandan secondary schools support older students as they transition toward adulthood.
The unseen influence of family mental health
The study also found that adolescents with a family history of mental illness had twice the odds of exhibiting behavioral problems compared to those without such a history.
“This speaks to the intersection of genetics and environment,” says Bobholz. “Living in a household with people affected by mental illness can mean instability, stigma, and lack of emotional support, all of which weigh heavily on a developing mind.”
The authors recommend that school mental health screening include family mental health history and advocate for greater collaboration between education and health sectors to support at-risk households.
Private schools: High marks, higher stress?
Interestingly, students in private schools had 1.4 times the odds of experiencing emotional disorders compared to those in public schools. Private schools, often seen as academic havens, may inadvertently be cultivating high-pressure environments. “There’s an assumption that better facilities mean better well-being,” says Dr. Abbo. “But intense academic competition, social isolation, and a lack of trained counselors can create emotional pressure cookers.”
Previous research in 47 secondary schools across five districts (Rakai, Kyotera, Masaka, Lwengo, and Kalungu) in southwestern Uganda found that economic and family support helped reduce absenteeism among adolescent girls in secondary schools. However, this support did not significantly improve behavior or reduce grade repetition. The region, which includes districts like Rakai and Masaka, also faces a higher burden of HIV, adding to the challenges young people experience.
Meanwhile, a review of data from 42 primary schools in Luwero District identified school-based mental health interventions such as cognitive behavioral therapy and mindset-building approaches as being particularly effective. Researchers now suggest that integrating these strategies, along with efforts to reduce school violence, could go a long way in improving the mental health of Ugandan adolescents.
A-Level pressure: Academic ambition meets mental health strain
The study also found a correlation between advanced (A’level) education and increased risk of emotional disorders. “We selected one school district from each region based on population and past academic performance. As these students prepare for university or the job market, the pressure to succeed becomes enormous,” says Kasasa. “They’re facing a future full of uncertainty, with very little structured mental health support to help them cope.”

A wake-up call for Uganda’s education and health systems
The authors of this study assert the urgent need for school-based mental health programs, especially in private and A-level institutions. These programs should offer routine screening, emotional support, and training for teachers to recognize warning signs of mental health disorders.
Importantly, this study adds weight to calls for a national adolescent mental health policy, tailored to Uganda’s context, with interventions that bridge health, education, and social services.
“Our data shows that mental health challenges are not a fringe issue,” says Bobholz. “They are widespread, significant, and deeply tied to school, home, and society.”
The COVID-19 school closures between 2020 and 2022 deepened feelings of isolation and financial strain, with out-of-school adolescents reporting depression rates as high as 21.5% to 50% higher than their peers who remained in class, according to research published in February 2025. Yet Uganda invests less than 1% of its health budget in mental health, with just one psychiatrist per million people, leaving many teens to cope through cheap alcohol used by 28% of urban youth or untrained healers, as reported by the government paper The New Vision in April 2025. With only 26% of students completing lower secondary school and 35% of the population under age 24, these mental health challenges now pose a serious threat to the country’s future.
Mercy Akankunda of Proven Foundation, a Ugandan NGO supporting vulnerable groups, warns that mental health struggles are quietly eroding the well-being of the country’s youth, over 12 million strong and making up 35% of the population. “These teens are not just statistics. They are the future of Uganda, she asserts. If Uganda hopes to reap the dividends of its young population, addressing adolescent mental health must become and remain a national priority, not just for treatment, but for prevention, resilience, and hope.
Reference:
Bobholz, M., Dickson-Gomez, J., Abbo, C., Kiconco, A., Shour, A.R., Kasasa, S., Cassidy, L.D., & Anguzu, R. (2025). Correlates of behavioral and emotional disorders among school-going adolescents in Uganda. PLOS Global Public Health. Read the study here
Health
Call for Applications: Responsible Conduct of Research (RCR) Training Course
Published
1 week agoon
July 11, 2025By
Mak Editor
The Responsible Conduct of Research (RCR) Training Course, scheduled to take place from July 30th to August 1st, 2025, at the Makerere University College of Health Sciences’ Conference Room.
Background
The SUSTAIN: Advancing Makerere University Masters of Health Sciences in Bioethics program at Makerere University College of Health Sciences aims at developing and institutionalizing a mentorship program in research ethics that facilitates development of bioethics professionals and health researchers who are committed to the growth and application of research ethics in Uganda’s academic and research institutions to the highest possible degree. The Responsible Conduct of Research (RCR) course is one of the short courses that introduces trainees to a framework that involves application of established scientific, professional norms and ethical principles in the performance of all activities related to scientific research.
Course objectives
At the end of this course, trainees should be able to identify, manage and prevent research misconduct.
Course outline
Introduction to RCR; Introduction to Professionalism and Ethics; Human subject’s protection and regulatory framework in Uganda; Humane handling of animal research subjects; Conflict of interest;
Responsible laboratory practices; Mentor-mentee relationships; Collaborative research international, industry); Peer review; Research misconduct (including policies for handling misconduct); Community involvement during research in a low resource setting; Responsibility to society and environment; Responsible financial management; Data acquisition, management, sharing and ownership; Responsible authorship, publication and communication.
Target group
The Responsible Conduct of Research course is targeted at Researchers, Research administrators, Research assistants, Study coordinators, Graduate students and Student supervisors. Certificates will only be awarded to participants with 80% attendance.
Course fee: 205,000/=, or 56USD is payable.
The course fee will cater for meals and refreshments during the training period.
Payment & Registration procedure:
9030026194023, Stanbic Bank, Mulago, Makerere University Biomedical Research Center Limited
Dollar Currency:
9030026194147, Stanbic Bank, Mulago, Makerere University Biomedical Research Center Limited
Please Note: Share payment details on email/whatsup and a hardcopy deposit slip delivered on the first day of the training to Miriam Musazi, Department of anatomy, Bioethics Centre, Room C4,
Mob: +256 782 363 996/ +256 701 363 996, Email: mmusazi@gmail.com.
NB. Only those who will have paid by this date will be considered for the course
Venue: The training will take place at Makerere University College of Health Sciences’ Conference room
Trending
-

 General2 weeks ago
General2 weeks agoRe-advert: Admission to Undergraduate Programmes 2025/2026
-

 General1 week ago
General1 week agoRe-Advert for Applications for Diploma and Certificate Training
-

 General5 days ago
General5 days agoMakerere University Fees Waiver for 40 First Year Female Students 2025/2026
-

 General2 weeks ago
General2 weeks agoPress Statement on Ranking
-

 Health1 week ago
Health1 week agoCall for Applications: Responsible Conduct of Research (RCR) Training Course
