Health
Makerere University Population Cohort (MUCHAP/IMHDSS) to conduct a Community Medical Camp
Published
3 years agoon
By
Mak Editor
MUCHAP, the Makerere University Centre for Health and Population Research, is dedicated to improving the well-being of the Ugandan population through the generation and dissemination of high-quality demographic, health, and socio-economic information. With a focus on the Iganga-Mayuge Health and Demographic Surveillance Site (IMHDSS), MUCHAP has been actively engaged in monitoring births, deaths, and migrations for over 15 years. By conducting impactful research that addresses community needs, MUCHAP aims to bridge the gap between academic research and the practical needs of households and individuals.

To further this mission, MUCHAP is organizing a health camp in Wairama trading centre, Nakigo sub-county, Iganga district on 17th June, 2023, starting at 9:00 AM. Building upon the success of a previous health camp in 2017, which collected over 700 units of blood and served more than 2,000 community members, this upcoming event aims to tackle the significant challenge of child mortality in the region. By raising awareness, improving access to healthcare services, and investigating the causes of child death, the health camp strives to enhance the overall health of the community.
The core objective of the community engagement, which includes a medical camp, is to bring the university’s research directly to the community, incorporating community voices and addressing their needs. Dr. Dan Kajungu, the Lead Research Scientist and Executive Director of MUCHAP, outlines the objectives of the medical camp.
“These include health education on topics such as childhood immunization, child and maternal health, health-seeking behaviors, personal and household hygiene, and early screening and diagnosis for non-communicable diseases like diabetes, cancers, and cardiovascular diseases.
“Additionally, the camp aims to provide feedback to the community regarding past research conducted and its implications for population well-being. Furthermore, the event will facilitate a dialogue on innovative technologies such as the minimally invasive tissue sampling (MITS) method for determining the cause of death, which involves conducting autopsies without fully opening the body” he said.
The health camp will also serve as an opportunity to sensitize and engage the community about the importance of registering all births and deaths with the National Identification and Registration Authority (NIRA) systems. Recognizing that many events, including those occurring within health facilities, often go unregistered in the Civil Registration and Vital Statistics (CRVS) system, the HDSS is collaborating with NIRA to enhance registration through community structures such as Village Health Teams (VHTs) and Local Council One Chairpersons. Leveraging their experience and expertise in community-level registration since 2005, MUCHAP aims to promote comprehensive CRVS coverage.
Looking ahead, MUCHAP envisions establishing a community research and public health laboratory that is accessible and community friendly. This laboratory will provide convenient services to community members while facilitating essential research, similar to centers in South Africa and other developed countries.

This endeavor is supported by the Makerere University Biomedical Research Center (MakBRC), which builds upon existing infrastructure that was partly funded by Pfizer International by contributing to the construction of the current center premises.
Working with healthcare workers from Iganga General Hospital and other community-based public health facilities, the health camp will offer a range of activities including community engagement, health education talks, screenings, and laboratory tests for common diseases. Community members will receive various products and services, such as treated mosquito nets, family planning services, medication, and immunizations for eligible individuals.
Through these initiatives, MUCHAP aims to empower the community with knowledge, resources, and improved access to healthcare, thereby addressing key health challenges and working towards a robust disease surveillance system at the community level.
You may like
-


Holding the System Together During COVID-19: Steven Kabwama’s Research on Care Continuity
-


Dr. Samalie Namukose and the Quiet Work of Making Nutrition Count
-

Call for PhD Student Fellowships under H-DATA
-


Simon Mungudit: Mak’s Best Performing Male Science Student & Rising Star in Petroleum Geoscience
-


Call For Applications: MakNCD Masters and PhD Training Opportunities
-


Press Statement: Makerere University Congratulates Former Staff and Students on Successful Election to Public Office
Health
Holding the System Together During COVID-19: Steven Kabwama’s Research on Care Continuity
Published
1 day agoon
February 6, 2026
In March 2020, Uganda slowed to a near standstill. Roads emptied. Clinics fell quiet. Fear moved faster than information. Many perceived COVID-19 as a virus to avoid. Others saw it as a barrier that stood between a mother and antenatal care, a child and routine immunization, and a patient and life-saving HIV medication. What followed was not only a public health emergency but also a test of whether health systems could keep doing the ordinary work of care while responding to the extraordinary.
In early December 2025, a question first asked with urgency during a global crisis resurfaced in a quieter, more reflective moment. On December 2, a single bound copy of Steven Kabwama’s doctoral thesis was fastened to a wooden board dubbed ‘The Wall of Fame‘ at Karolinska Institutet. The ritual, known as spikning, is modest in appearance but weighty in meaning: a thesis is made public, opened to scrutiny, and years of private intellectual labour are released into the world. For Kabwama, it marked the moment when research forged in the pressure of a global emergency became part of the public record, no longer his alone but open to collective examination.
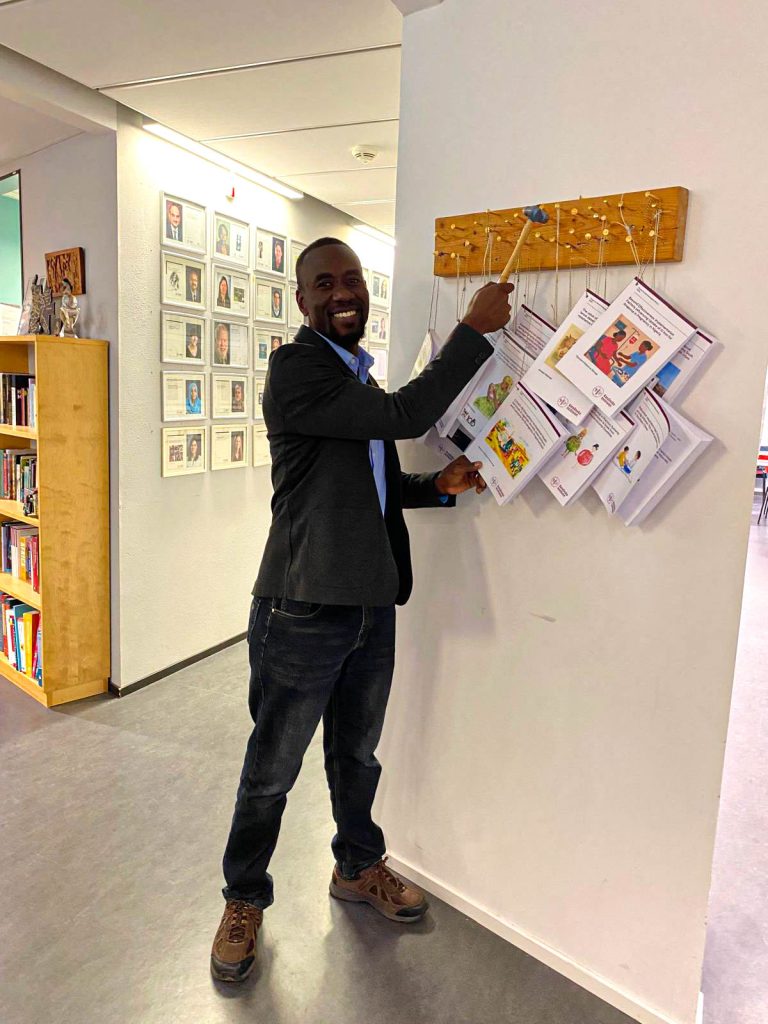
The tradition stretches back centuries, often traced to Martin Luther’s public posting of his theses in the 15th century. But in Stockholm, on a winter afternoon, history gave way to something more immediate. Kabwama stood briefly by the wooden board with a hammer and fixed his work in place. The moment was less about ceremony than readiness. The research was complete. The questions were now open.

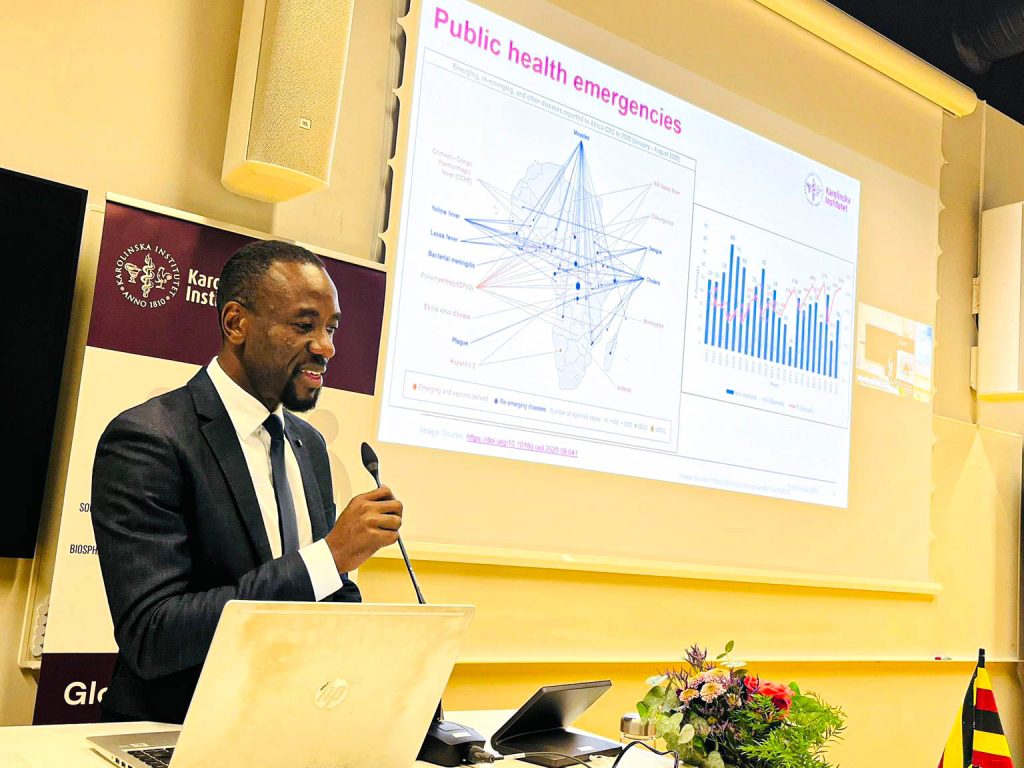
Three days later, on Friday, December 5, 2025, Kabwama publicly defended the thesis in a hybrid ceremony at Wretlindsalen in Solna, joined, both in person and online, by colleagues from Uganda, Sweden, and beyond. By then, the work, which examines how health systems sustain essential services during crises, had already begun to circulate, quietly shaping conversations about preparedness, continuity, and care.

What that bound document contained, however, had been forged years earlier, inside outbreaks, lockdowns, data sets, and long nights spent asking how health systems hold together when everything else is falling apart.
Steven Ndugwa Kabwama remembers the beginning not as a single crisis, but as a series of decisions, some made urgently, others too late. As an epidemiologist by training, Kabwama, who had spent years responding to outbreaks through Uganda’s Field Epidemiology Fellowship Program, clearly understood that outbreaks had patterns; they arrived, demanded attention, and eventually receded.
COVID-19 was different.
“It became clear very early on,” he recalls, “that the urgency of the response was going to affect everything else: malaria, immunization, maternal health, HIV. And yet, very little had been written about how systems are supposed to hold both at the same time.”
That realization would shape the next chapter of his life and, eventually, his PhD.
From Outbreak Response to System Questions
Kabwama’s academic journey did not begin in epidemiology. In 2006, he enrolled for a Bachelor’s degree in Food Science and Technology at Makerere University, a programme traditionally geared toward food processing, quality assurance, and industrial production. It is a discipline that prepares graduates for careers in manufacturing plants, laboratories, and supply chains, work that often unfolds far from clinics, outbreaks, and emergency response rooms.
Yet even then, his interests leaned beyond production lines and quality controls. He was drawn to how systems affect people’s health long before illness appears and how nutrition, safety, access, and policy intersect. That early grounding in systems thinking would later resurface in unexpected ways.
He went on to earn a Master of Science in Public Health from the University of Southern Denmark in 2013, supported by a Danish State Scholarship. It was there that population-level analysis sharpened his interest in data, surveillance, and health equity. But it was the Advanced Field Epidemiology Fellowship, jointly run by Makerere University School of Public Health (MakSPH), Uganda’s Ministry of Health, and the U.S. Centers for Disease Control and Prevention, that placed him directly inside emergencies, where evidence, decisions, and lives converge.
As a Fellow, his work stood out. He later received the Outstanding Fellow Award from the Uganda Public Health Fellowship Program (Field Epidemiology Track, Cohort 2015), recognition of his contributions to outbreak response, national non-communicable disease analyses, and policy work, including Uganda’s Alcohol Control Policy. “You respond, you stabilize, you move on,” he says. “But I kept asking myself—what happens to everything else while we’re responding?”

The arrival of COVID-19 made it impossible to delay these questions.
A Crisis Within the Crisis
As countries rushed to contain the virus, restrictions came swiftly: lockdowns, curfews, and travel bans. From a disease-control perspective, the logic was familiar and defensible. In outbreak management, 21 days is a standard epidemiological window, often used to break chains of transmission in infectious diseases. But during COVID-19 in Uganda, the phrase “therefore…another 21 days of lockdown” took on a different meaning altogether: The repeated phrase in presidential addresses stretched from a technical containment tool into a lived reality that reshaped access to care, livelihoods, and movement. From a health-system perspective, the consequences were profound.
Kabwama joined a multi-country research effort spanning Uganda, Nigeria, the Democratic Republic of Congo, Senegal, and Ghana, examining how countries attempted to maintain essential health services while responding to COVID-19. This work was spearheaded by Dr. Rhoda Wanyenze, a Professor of Disease Control, Researcher, Public Health Expert, and Dean of the School of Public Health at Makerere University. She was then a member of the COVID-19 Scientific Advisory Committee to the Ministry of Health.
Kabwama volunteered to lead the objective of documenting these experiences, an area he quickly realized was underexplored.
“Criticism is always easier in hindsight,” he reflects. “But generally, the considerations about how restrictions would affect access to essential health services were made after the fact.”
His doctoral research, later defended at Karolinska Institutet, set out to answer a deceptively simple question: How can health systems minimize disruptions to essential services during public health emergencies while emerging stronger afterward?

What the Data Revealed
Kabwama examined how health service use changed before and during the pandemic by using a mix of interrupted time-series analysis, document reviews, key informant interviews, and focus group discussions.
The findings were sobering.
Facility deliveries and outpatient visits dropped sharply during lockdown periods. Routine childhood immunizations declined, and DPT3 doses fell by more than 4 percent, with similar reductions across polio vaccines. Movement restrictions, fear of infection, and overwhelmed facilities combined to keep patients away.
But the story did not end there.
Where systems were adapted by integrating services, leveraging community health workers, removing user fees, modifying logistics, and establishing coordination mechanisms for continuity of care, the declines softened. In some cases, the adaptations strengthened systems beyond their pre-pandemic state.
“These were not perfect solutions,” Kabwama notes. “But they showed us what flexibility, leadership, and trust can do under pressure.”
The Human Cost—and the Human Shield
Behind every data point were health workers navigating impossible conditions. Many worked without adequate protective gear. Others faced delayed allowances, long hours, and constant risk.
Kabwama asserts that health workers risk their lives in their work. “If we expect services to continue, then protecting their physical and mental well-being is not optional.”
His research consistently returned to one conclusion: that service continuity depends on people. Policies can guide. Infrastructure can support. But without motivated, protected health workers and trusted community intermediaries, systems falter.
Uganda’s community health workers, he observed, became a backbone of resilience. They traced contacts, delivered information, encouraged women to attend antenatal care, and helped sustain immunization demand when facilities felt distant or dangerous.
“In our context,” he says, “they were critical. That’s a lesson worth holding onto.”
Learning Across Borders
Conducting his PhD through a collaborative programme between Karolinska Institutet and Makerere University School of Public Health exposed Kabwama to how different systems responded under pressure.
At Karolinska’s Department of Global Public Health, students from around the world shared experiences shaped by culture, trust, and governance. One story stayed with him: Sri Lanka’s military, highly trusted by the public, played a key role in vaccine rollout.
“It taught me that resilience looks different everywhere,” he says. “What matters is understanding what each system already has and how trust operates within it.”
His supervision team, spanning Sweden and Uganda, including Prof. Tobias Alfvén, Prof. Rhoda K. Wanyenze, Dr. John Ssenkusu, Prof. Helena Lindgren, and Dr. Neda Razaz, reflected that same cross-system thinking.
Wanyenze describes Kabwama as “focused, committed, and remarkably productive.” She notes that he led two major workstreams across the five participating countries, helping generate critical evidence on health systems resilience and trust during infectious disease emergencies. “He made an enormous contribution to the research,” she says, “and he continues to do excellent work in this area.”
The Quiet Challenge of Doing Research in a Pandemic
Methodologically, the pandemic forced adaptation. Interviews moved to phones and Zoom. Access was negotiated carefully. Yet Kabwama sees the technology not as a limitation but as a strength.
“We captured experiences while they were still fresh,” he explains. “Before details were forgotten, before narratives were smoothed over.”
That immediacy gave his work an unusual clarity, documenting decisions as they unfolded, not as they were later remembered.
But beyond COVID-19, Kabwama’s thesis does not treat it as an anomaly. Rather, it presents COVID-19 as a stress test, exposing pre-existing weaknesses and potential strengths.
His central argument is that the ability to maintain essential health services during emergencies depends on baseline capacity.
“Now is the time,” he says, “to invest in health workers, in infrastructure, in guidelines for service continuity. This should be done now, not when the next crisis arises.
That conviction extends to learning itself. After-Action Reviews are conducted, lessons are noted, but too often, they fade.
“We need to be deliberate about learning,” he insists. “About documenting what worked and making sure those gains are not lost once the emergency ends.”
Work That Continues
Today, Kabwama is a Research Associate at Makerere University School of Public Health, a Monitoring, Evaluation and Learning Specialist with the Uganda Public Health Fellowship Program, and a member of WHO initiatives on trust and pandemic preparedness. He leads mortality surveillance in Uganda’s island districts, supports national NCD analyses, and continues to advise on emergency preparedness across Africa.

He remains, by his description, an optimist.
“There are people who think we are worse off now than before COVID-19,” he says. “In some ways, that’s true. But there are also many ways in which we are better prepared.”
Vaccines, data systems, community engagement, and global awareness have all shifted. The challenge is ensuring that momentum does not fade.
Dr. Steven Ndugwa Kabwama joins fellows in the MakSPH PhD forum who concluded their doctoral journeys in 2025. And the work of his research and scholarship does not promise certainty but offers something more useful: evidence that systems can bend without breaking—if they are prepared to learn, invest, and protect the people who hold them together.
Health
Dr. Samalie Namukose and the Quiet Work of Making Nutrition Count
Published
1 day agoon
February 6, 2026
Between Tuesday, February 24 and Friday, February 27, 2026, Freedom Square at Makerere University will fill with a familiar choreography of anticipation. The air will fill with the rustle of academic gowns, the nervous laughter of graduands, and the careful positioning of proud families searching for familiar faces in a sea of crimson, green, and black. It is a moment of ceremony, yes, but also of reckoning.
Up close, the doctoral gowns feel heavier than they look. The deep crimson fabric, warm and deliberate, settles on the shoulders. Green panels edged in gold are gently pressed against the chest. Wide sleeves gently brush against clasped hands, soft bonnets rest low on foreheads, and tassels remain motionless. Beneath the regalia are steady breaths, quickened heartbeats, and bodies carrying the quiet fatigue of years spent balancing work, study, and life. These are garments worn not only for display but also for endurance, stitched to nights without sleep, to questions carried long before they were answered.
At this four-day Makerere University’s 76th Graduation Ceremony, 185 doctoral degrees will be conferred. Each PhD will represent years of unanswered questions, interrupted sleep, financial strain, and relentless intellectual persistence. Among them will be Dr. Samalie Namukose, a woman whose academic journey was never separate from the health system she serves, only threaded through it.
For more than two decades, Samalie Namukose has worked inside Uganda’s Ministry of Health, rising steadily from Nutritionist to Assistant Commissioner for Health Services/Nutrition. She has helped write policy, coordinate national programs, supervise districts, respond to emergencies, and advocate for mothers and infants whose voices rarely travel beyond clinic walls. Her PhD did not pull her away from that world but plunged her deeper into it.

The Question That Would Not Let Go
Dr. Namukose’s doctoral journey began not in a library, but in a pattern she kept seeing and could no longer ignore.
Uganda’s nutrition policies are robust. They speak clearly about the importance of maternal and infant nutrition, especially in the first 1,000 days of life. Yet in health facilities across the country, nutrition services often appeared fragmented, present in principle, and inconsistent in practice. Mothers attending antenatal or postnatal care were weighed, yes, but not always counselled. Infants were measured, but follow-up was irregular. Nutrition existed, but it was not always integrated.
“I kept asking myself,” she recalls, “not whether nutrition interventions exist, but how well they are embedded in routine care, and what prevents health workers from delivering them consistently.”
That question shaped her PhD research at Makerere University’s School of Public Health, where she examined the integration of Nutrition Assessment, Counselling, and Support (NACS) into routine health services in the Tororo and Butaleja districts in Eastern Uganda.
At its core, NACS integration is deceptively simple: assess nutritional status at every health point, provide tailored counseling, and link clients to support within the same system and beyond. But in practice, it tests the very backbone of health systems: workforce capacity, financing, governance, supervision, and community linkages.
“When NACS is well integrated, health facilities can identify nutrition risks early, prevent deterioration, and provide timely support rather than responding only when malnutrition becomes severe,” she says.
Inside Resource-Constrained Health Facilities
What Dr. Namukose found was not a clear story of failure or success, but something in between. Many health facilities were offering basic nutrition education and assessments, and health workers were clearly trying their best. However, long patient queues, limited time, and a shortage of basic tools and job aids often hindered counseling and follow-up. Food demonstrations were rare. Growth monitoring was inconsistent. Efforts to improve quality occurred only sporadically.
In facilities without trained nutritionists, nurses, and midwives, already stretched thin, took on nutrition work alongside many other duties, leaving little room to support mothers and children in a steady, continuous way.
And yet, her findings revealed something deeply hopeful: “facilities with knowledgeable, motivated, and supported health workers delivered better nutrition services, even within the same constraints.” To Dr. Namukose, this showed that leadership, mentorship, and attitude mattered. Where nutrition was treated not as an extra task but as essential care, outcomes began to improve.
One of the strongest findings from Dr. Namukose’s research was that even when nutrition services were only partly integrated, they still made a visible difference. Mothers gained weight more steadily during pregnancy and in the early months of breastfeeding. Babies were born heavier and grew better in their first months of life. Across health facilities with more fully integrated nutrition services, children consistently showed healthier growth patterns.

These were not just numbers on a page; babies started life stronger, and mothers were better supported to care for them.
“To me,” she explains, “the improvements in maternal weight gain reflected the value of regular assessment and context-specific counseling. For infants, the better growth outcomes showed that a package of nutrition interventions, delivered consistently, can make a real difference during the most critical window of life.”
It was clear evidence that nutrition integration works effectively, though gradually and significantly.
The Fragility of Progress
Dr. Namukose’s research also exposed how fragile these gains remain. Weaknesses in financing and governance emerged as the greatest threats to sustainability. Nutrition services often depended on unpredictable partner funding rather than routine government budgets. Essential supplies, anthropometric tools, job aids, and therapeutic foods were frequently unavailable or externally dependent.
Her study captured glaring governance gaps that compounded the problem. For instance, nutrition was not always clearly positioned within accountability structures, and this, according to Dr. Namukose, often led to limited supervision and weak performance monitoring. Many districts lacked dedicated nutritionists altogether.
She notes that community follow-up was essential for sustaining behaviour change after clinic visits, especially for those who suffered most. Village Health Teams and care groups struggled without supervision, feedback mechanisms, or resources.
“Most nutrition-related behaviours, such as maternal diet, infant and young child feeding, and care practices, are shaped and sustained within households and communities,” says Dr. Namukose.
She contends that nutrition integration cannot rely on projects but must be embedded in systems.

A PhD Written in the Margins of Life
Conducting this research while holding a senior national leadership role in the Ministry of Health was, by her own admission, one of the hardest things she has ever done.
Dr. Namukose did not request study leave. Partly self-sponsored, she worked full days at the Ministry of Health, then wrote at night, often between midnight and 4:00 am, and again in the early mornings, on Saturdays, and on borrowed hours of Sunday.
“There were days when I sacrificed sleep completely,” she says quietly.
National emergencies such as COVID-19, Ebola, and MPOX repeatedly interrupted her doctoral journey, drawing her back into crisis response. To her, returning to her PhD after each interruption felt like re-entering a conversation mid-sentence, struggling to find the thread.
At one point, she simultaneously prepared for a Top Management Committee presentation, attended a doctoral committee meeting, and sat for Health Service Commission promotional interviews.
“The pressure from the supervisors kept me on my toes. The PhD forum was another motivating factor, consistently sharing updates, books, courses, encouragement, and invitations to PhD defenses. Peer support was tremendous. Without a supportive family, you can’t make it,” she remarks.
A Career That Prepared the Ground
Dr. Namukose’s PhD sits atop a formidable professional foundation. She holds Bachelor’s and Master’s degrees in Agriculture from Makerere University, a Postgraduate Diploma in Food and Nutrition Security from Wageningen University in the Netherlands, and a Postgraduate Diploma in Business Administration from Makerere University Business School. She has undergone extensive training in nutrition leadership, research methods, health systems, and quality improvement across Africa, Europe, and Asia.
Within the Ministry of Health, she has served as a Public Health Nutritionist, Senior Nutritionist, Principal Nutritionist, and now Assistant Commissioner, coordinating national nutrition interventions, designing training modules, mobilising resources, and overseeing district implementation.
She has played key roles in multi-million-dollar initiatives, from HIV-Free Survival programmes to Integrated Child Health Days, public food procurement policy, and the scale-up of Multiple Micronutrient Supplements (MMS) for pregnant women.
Her research has been published in leading peer-reviewed journals, including PLOS ONE and BMC Health, Population and Nutrition, ensuring that her findings speak both to policy and global evidence.
On a mission to keep research from gathering dust
Now a Doctor of Philosophy, Dr. Namukose has determined that her work will not sit quietly on a shelf. Her findings have already informed Uganda’s Health Sector Nutrition Strategic Plan, strengthening the case for financing, governance reform, and recruitment of skilled nutrition cadres. She continues to champion platforms, such as national nutrition symposia, that bring student research into policy dialogue and implementation spaces.
“Very often, excellent student research is left on the shelves. I plan to allocate some days during these symposia to nutrition students to showcase best practices and innovations,” she says.
Adding that, “I urge mothers and their infants to actively engage in self-care, growth-promotion, and monitoring activities to improve their own health and that of their children.”
Central to her recommendations is a call to embed nutrition services within routine health and community systems, with sustained government leadership, financing, and competent human resources.
Integration, she insists, is not achieved by guidelines alone, but through continuous engagement with frontline health workers and communities.
As graduation day approaches, Dr. Namukose’s thoughts turn outward. To frontline health workers delivering nutrition services under pressure, her message is one of respect and reassurance. Even with limited resources, the assessments they conduct, the counselling they provide, and the care they offer can change outcomes.
“Endeavor to participate in training programmes whenever available to bridge gaps in nutrition knowledge and skills, including on-the-job and rotational training to support cost-effective and efficient nutrition service delivery,” she asks.
To mothers and caregivers, she urges active engagement in self-care, growth monitoring, and nutrition programmes, especially those strengthened through digital innovation.
And to policymakers, her research offers both evidence and urgency that nutrition integration is no longer optional but foundational to maternal and child health.

When Dr. Samalie Namukose walks across the stage at Freedom Square, followed by applause, the true weight of that moment lies in health facilities where nutrition is no longer an afterthought. In mothers whose pregnancies are better supported. In infants whose growth curves bend upward, quietly, decisively.
Among the 185 PhDs conferred at Makerere University’s 76th graduation, the School of Public Health Communications Office shares her story, which is a reminder that the most transformative scholarship is not always loud. It builds patiently, between policy meetings and midnight writing, between emergencies and examiners’ comments, until it transforms systems and lives from within.
Health
EU Earmarks Shs19.8bn for 15 Joint PhD Scholarships in Health, Environment Research
Published
4 days agoon
February 3, 2026By
Zaam Ssali
By Violet Nabatanzi & Zaam Ssali
The European Union has earmarked Euros 4,658,684 approximately (Shs19.8 billion) to fully fund 15 PhD scholarships under a new international collaborative research programme that brings together seven universities across Africa and Europe, including Makerere University.
The project, dubbed HEALENAE (Health and Environment in Africa and Europe), will support doctoral research examining the complex links between environmental change, climate crises and health outcomes, with a strong focus on Africa Europe comparative perspectives.
The scholarships are open to anthropologists, social scientists and related humanities scholars who hold an internationally recognised Master’s degree and are interested in pursuing a joint PhD (dual degree).
Dual degrees across continents
Successful candidates will be enrolled at two universities one in Africa and one in Europe and will graduate with a joint or dual PhD degree. The consortium brings together Makerere University, University of Oslo, University of Cape Town, KU Leuven, University of Edinburgh, University of Nairobi, and Aarhus University.
The PhD research areas include:
- Metabolic impact: agricultural intensification and health transformations
- Climate change migration and care for the elderly.
- Toxic layering in a precarious world: environmental harms and well-being.
- Livestock and natural resource management: biodiversity and zoonotic diseases.
- Epidemics, disease and state formation in Africa.
- Climate crisis, youth migration, adaption and associated health outcomes.
- Toxicity: urban living in landscapes of extraction.
- Gendered cancer epidemics and questions about environments
- Infrastructures of toxic evidence and civic protection
- Biosecurity: food, health risks and animal disease.
- Non Communicable Diseases, environments and questions of repair.
- Urban commons: environments, infrastructures, and health.
- Youth mental health and gambling epidemics in times of environmental crisis.
- Epidemics and natural disasters as ‘business’.
- The Frontiers of Vector Borne Disease: Expertise and Response in Africa and Europe.
Dr. Godfrey Siu, the University’s Senior Lecturer and Director of the Child Health and Development Centre (CHDC); Dr. Herbert Muyinda, Senior Lecturer; Prof. Stella Neema from the Department of Sociology and Anthropology; alongside Prof. Lotte Meinert of Aarhus University will jointly supervise the students, together with other PhD supervisors from other collaborating Universities.
On Tuesday, January 27, Prof. Julius Kikooma, Director of the Directorate of Graduate Training at Makerere University, Dr Siu, Dr Muyinda, and Prof. Neema alongside Prof. Lotte paid a courtesy visit to the University’s Vice Chancellor, Prof. Barnabas Nawangwe.
Prof. Nawangwe welcomed the funding and commended the EU for its support, noting that the generous contribution reflects the confidence the EU has in Makerere University. He added that the University is working hard to address the loophole previously raised by the EU regarding the implementation of EU-funded grants. The Vice Chancellor congratulated the team and pledged the University’s full support to ensure the project’s successful implementation.
Who should apply
Speaking in an interview, Prof. Lotte said the program is particularly suited for candidates with strong grounding in anthropology, sociology and related social sciences.
Eligible candidates must have an internationally recognised Master’s degree in anthropology or related social sciences and humanities disciplines.
Lotte added that the positions are fully funded for three years, with generous support for fieldwork, coursework, conferences, writing retreats and research training.
Candidates are expected to conduct up to 12 months of fieldwork. They will be enrolled at both universities and are required to spend at least one semester at the partner institution.
A first for Uganda
According to Dr Siu, the HEALENAE model where fifteen joint PhDs are funded under one programme is the first of its kind in Uganda.
Addressing concerns about differing academic expectations across universities, Dr Siu said these are anticipated and manageable.
“While there are some differences, PhD training globally follows a similar structure. For instance, Makerere requires all PhD students to complete mandatory cross-cutting courses, including philosophy of methods, advanced research methods, and scholarly writing and communication skills,” he said.
In addition, students will attend writing retreats and specialised training schools, some of which will be hosted at Makerere University and the University of Nairobi, aimed at sharpening their research and analytical skills.
Prof. Kikooma briefed the team on the structure of the PhD program at Makerere University and provided guidance on how to align the dual program with the University’s framework.
He also pledged his support and expressed optimism that the program offers new opportunities for Makerere University to learn from and strengthen dual programs. The initiative aligns with Makerere’s vision of becoming a research-led university through intensified PhD training.
Application deadline
Interested candidates are encouraged to visit the HEALENAE website for detailed calls and application guidelines. The deadline for applications is March 1, 2026.
The application link is provided below.
https://phd.arts.au.dk/applicants/open-and-specific-calls/healenae-project-2
For further information contact: godfrey.siu@mak.ac.ug
Trending
-

 General2 weeks ago
General2 weeks agoPress Statement: Makerere University Congratulates Former Staff and Students on Successful Election to Public Office
-

 General1 week ago
General1 week agoPress Statement: Makerere 76th Graduation Ceremony
-

 General4 days ago
General4 days agoCall for Applications: Admission to Postgraduate Programmes 2026/2027
-

 Natural Sciences4 days ago
Natural Sciences4 days agoSimon Mungudit: Mak’s Best Performing Male Science Student & Rising Star in Petroleum Geoscience
-

 Health6 days ago
Health6 days agoCall For Applications: MakNCD Masters and PhD Training Opportunities
