Health
Mak’s Findings: Index Patients Diagnosed and Treated for COVID-19 in Uganda
Published
6 years agoon

On Tuesday May 26, 2020, Makerere University (Mak) Management converged to share findings from the study whose aim of was “to detail characteristics and treatment outcomes of the Coronavirus (COVID 19) pandemic patients in Uganda”. Coronavirus being a novel and rapidly changing pandemic, it was essential that early lessons are obtained and synthesised. These lessons directly feed into the clinical care guidelines and eventually contribute to the country’s interventions. With funding from the Government of Uganda through the Makerere University Research and Innovations Fund (Mak-RIF), this study was successfully executed.The multidisciplinary research team was coordinated through the Makerere University Lung Institute (MLI) http://mli.mak.ac.ug/. This study was led by Dr. Bruce Kirenga, Director MLI, and Prof. William Bazeyo, Acting Deputy Vice Chancellor (Finance and Administration)-Mak as Principal Investigators. Other investigators were from Entebbe Regional Referral Hospital, Johns Hopkins University, Baltimore, USA, Uganda Peoples Defence Forces, The AIDS Support Organisation (TASO), Mulago National Referral Hospital, the College of health Sciences and Ministry of Health, Uganda.
This study was conducted on the first group of COVID-19 patients (56) at Mulago National Referral hospital and Entebbe Regional Referral hospitals. Patient enrolment has continued but below we exultantly share preliminary findings.
· Age: the average age of the patients in Uganda was 33 years which is far lower than has is reported elsewhere. In Wuhan China, for example, the average age is 59 while in the New York USA it is as higher (63 years). Older the patient have higher risk of severe forms of disease and ultimately the poorer treatment outcomes.
· Patient Presentation: Among symptomatic COVID-19 patients, the most common symptoms were fever (21.4%), cough (19.6%), runny nose (16.1%), headache (12.5%), muscle aches (7.1%) and fatigue (7.1%). However, more than half of the patients did not have any of these symptoms at diagnosis. These patients were largely travellers returning from abroad or contacts of the confirmed/symptomatic patients above. Unlike our patients, 80% of hospitalised patients in the western world were symptomatic.
· Laboratory and imaging tests: Coronavirus has been reported to affect almost all body tissues. To understand the extent of damage, our research team performed a wide range of tests including complete blood count, kidney function tests, troponin, lactate dehydrogenase which identifies for signs of damage to a wide range of body tissues, and C reactive protein-CRP. We found that 10.6% of the patients had low white blood cells, 26.3% had low platelets, and 12.8% had evidence of liver damage, while the kidneys had no evidence of damage. 12.2% had evidence of systemic inflammation and 43% had evidence of nonspecific tissue damage. The electrical heart activity was also checked with the electrocardiograph (ECG). All patients had normal ECG with the exception of one who had a very slow heart (bradycardia). We checked lung damage with Chest X-rays (CXR) and computed Tomography scans (CT). Three patients had significant lung damage on CT and CXR; while one of them had low oxygen saturation.
· Comorbidity: About 25% of the initial patients (56) reported having other medical conditions in addition to COVID-19. Most of the conditions reported were the non-communicable diseases such as hypertension and diabetes which accounted for 11%. High blood pressure (higher than 140/90mmHg) was the most common comorbid disease recorded in up to 28% of the patients.
· Disease severity: At admission, only 2 patients met the classification of severe disease (patients with severe respiratory symptoms requiring oxygen therapy) while the rest had mild disease. Temperature and oxygen saturation were monitored three times a day. All the patients recovered without the need for admission to Intensive care unit (ICU) or ventilation. This is contrary to what has been observed elsewhere, where 5% of COVD-19 patients required ICU care.
· Treatment: To-date, there is no known cure for COVID-19. The current treatments are meant to alleviate symptoms while waiting for the body to mount an immune response to fight off the infection. The patients were able to recover on supportive care through managing the symptoms, treatment with antibiotics for those who had evidence of bacterial infection, hydroxychloroquine and vitamin C. In instances where the patients had comorbid conditions, proper management of these conditions was part of the treatment.
Conclusion: The initial group of COVID-19 patients diagnosed in the country presented with mild disease and exhibited a clinical course of disease that is quite different from what has been observed elsewhere. Imaging and laboratory tests are critical in management of this disease. Prompt identification of patients and initiation of treatment could help to prevent the development of severe forms of the disease. Frequent monitoring of the oxygen saturation is also critical for rapid patient identification and treatment. In light of the increasing number of cases in the country, these findings help in informing the national preparedness plan for COVID-19 (capacity building of health workers in clinical care for COVID-19, the required logistics, continuous research).
Recommendations
1. Expand testing for COVID-19 in view of the finding that almost half of those confirmed did not have the classical symptoms for COVID 19. Add rhinorrhoea to symptoms for case screening.
2. Efforts should be taken to make clinical, laboratory and imaging tests available at all COVID-19 treatment centres to support proper grading of disease severity. At a minimum, pulse oximetry should be routine in management of COVID patients.
3. Capacity to diagnose and treat non communicable comorbid conditions should be built across the country as part of COVID 19 response. Equipment for proper diagnosis of these diseases should be secured, installed and effectively used.
4. Strengthen monitoring, evaluation and learning as part COVID-19 care. This will allow continued learning of COVID-19 in general and the effectiveness of the different treatments of the disease.
5. Research should be supported including biomedical sciences research. This will allow growth of locally generated evidence to support the country’s COVID 19 response.
Acknowledgement
· The Government of the Republic of Uganda, Makerere University Research and Innovations Fund (Mak-RIF), Ministry of Health, Uganda, Uganda Virus Research Institute, Mulago National Referral Hospital, Entebbe Regional Referral Hospital.
· The study participants, all health workers engaged and Makerere University leadership.
You may like
Health
MakCHS Strengthens Internationalization through Strategic Global Partnerships and Mobility
Published
4 days agoon
December 30, 2025By
Zaam Ssali
Makerere University College of Health Sciences (MakCHS) continues to advance its internationalization agenda by strengthening cross-border partnerships and expanding student and staff mobility in response to global health training needs. Recognizing international collaboration as a cornerstone of contemporary health professional education, the College has established strategic partnerships with leading institutions, including the University of the Western Cape (South Africa), the Medical University of Graz (Austria), and Universitas Syiah Kuala Faculty of Medicine (Indonesia). These collaborations focus on joint research initiatives and the training of dentists and physicians.

During the period July–September 2025, MakCHS recorded increased inbound student mobility, hosting 86 short-term international students. The majority (73%) came from eight partner institutions, with Europe accounting for 64% of all inbound students. Norway led with students from the University of Bergen and the University of Agder, followed by Italy and the Netherlands. The College also hosted students from Somalia International University, Moi University (Kenya), and institutions in the United States. Most visiting students were medical trainees, with placements mainly in Paediatrics at Mulago National Referral and Teaching Hospital, as well as Emergency Medicine and Obstetrics & Gynaecology at Kawempe National Referral Hospital.

These exchanges demonstrated strong bilateral commitment, notably with the Medical University of Graz, which sent students to MakCHS while simultaneously hosting MakCHS students, even in the absence of Erasmus Mundus Plus funding. Inbound mobility enriched the learning environment through intercultural exchange, inclusiveness, and exposure to diverse clinical and academic perspectives.

Outbound mobility also expanded significantly. MakCHS students undertook clinical rotations in the United Kingdom, the United States, and Austria. Two students completed hematology and oncology rotations at Addenbrooke’s Hospital, Cambridge, while others trained in plastic and reconstructive surgery at the University of Minnesota Medical Center–Fairview. Additional students undertook highly specialized rotations in paediatric surgery, orthopaedics, neurosurgery, and cardiac surgery at the Medical University of Graz, gaining exposure to advanced, patient-centred healthcare systems and strengthening their global clinical outlook.

Staff outward mobility was equally notable. Several MakCHS staff and graduate students participated in the Annual Global Health Conference organized by NUVANCE Health, an international partner. MakCHS faculty contributed through presentations, posters, and panel discussions, highlighting research on decolonization in global health education, adolescent health, and global mental health. These engagements provided valuable networking opportunities with global health funders and reinforced the importance of transnational academic partnerships in advancing health equity.

Through sustained partnerships, increased mobility, and active global engagement, MakCHS continues to position itself as a key contributor to global health education, research, and practice.
Health
Makerere University and Tsinghua University Launch Landmark China–Uganda Joint Laboratory on Natural Disaster Monitoring and Early Warning
Published
2 weeks agoon
December 19, 2025
Makerere University has taken a decisive step in strengthening Uganda’s and Africa’s capacity for public safety, disaster preparedness, and climate resilience with the official launch of the China–Uganda Belt and Road Joint Laboratory on Natural Disaster Monitoring and Early Warning, a flagship collaboration with Tsinghua University of China.
Launched during the Makerere University–Tsinghua University Symposium on Public Safety and Natural Disaster Management, the Joint Laboratory positions Makerere as a continental hub for cutting-edge research, innovation, and policy-relevant solutions in disaster risk reduction, early warning systems, and emergency response. The Laboratory will be hosted by Makerere University and is the only facility of its kind in Africa under this cooperation framework, underscoring its regional and global significance.
A Strategic Partnership Rooted in Research, Policy, and Practice
In his opening remarks, Prof. Barnabas Nawangwe, Vice-Chancellor of Makerere University and Ugandan Co-Director of the Joint Laboratory, traced the origins of the partnership to 2018, when a Makerere delegation visited Tsinghua University and the Hefei Institute for Public Safety Research. He recalled being deeply impressed by China’s advanced capacity in public safety research, disaster monitoring, and emergency management capabilities that directly respond to Uganda’s growing exposure to floods, landslides, epidemics, and other hazards.
The Vice-Chancellor noted that the successful establishment of the Joint Laboratory followed a competitive grant process under China’s Belt and Road Initiative, supported by the Government of Uganda and regional partners, including Nigeria and Côte d’Ivoire. He emphasized that the Laboratory aligns squarely with Makerere’s strategic ambition to become a research-led and research-intensive university, while also advancing its internationalisation agenda.

“This Laboratory will significantly enhance Makerere University’s ability to generate evidence-based research that directly informs government policy and public safety interventions. It will serve not only Uganda, but Africa at large,” Prof. Nawangwe said.
He further underscored the Laboratory’s national importance, noting that similar facilities in China are regarded as national-level laboratories, entrusted with supporting government decision-making and national resilience. Relevant Ugandan institutions, including the Office of the Prime Minister (OPM), UPDF, Uganda Police, Ministry of Health, and humanitarian actors, are expected to actively participate in the Laboratory’s work.
Tsinghua University: Advancing Science Diplomacy and South–South Cooperation
Speaking on behalf of Tsinghua University, Prof. Yuan Hongyong, Dean of the Hefei Institute for Public Safety Research and Chinese Co-Director of the Joint Laboratory, described the initiative as both a scientific milestone and a powerful demonstration of South–South cooperation.
He emphasized that natural disasters transcend national borders and demand collective, science-driven responses. By combining Tsinghua’s technological expertise, including satellite monitoring, AI-driven analytics, and integrated early warning systems, with Makerere’s deep regional knowledge and policy engagement, the Joint Laboratory provides a robust platform for innovation, applied research, and practical solutions tailored to African contexts.

The Laboratory will function not only as a research centre, but also as an operational platform for natural hazard monitoring, early warning, risk assessment, and capacity building, supporting Uganda and the wider African region in building more resilient communities.
Government of Uganda: Research as a Pillar of National Resilience
Representing the Office of the Prime Minister, Mr Frederick Edward Walugemba, reaffirmed the government’s strong support for the Joint Laboratory, recognizing research as a cornerstone of effective public safety and disaster management. The OPM highlighted its constitutional mandate to coordinate disaster preparedness and response through institutions such as the National Emergency Coordination and Operations Centre (NECOC).
He mentioned that the Office of the Prime Minister is committed to working closely with Makerere University and its partners, underscoring the importance of multi-agency collaboration, robust data systems, and timely policy advisories to address the complex, multidimensional nature of public safety challenges.
China–Uganda Relations and the Role of Science Diplomacy
Mr. WANG Jianxun, Commercial Counsellor of the Embassy of the People’s Republic of China in Uganda, lauded the Joint Laboratory as a concrete outcome of the growing China–Uganda Comprehensive Strategic Partnership. He emphasized that the collaboration reflects China’s commitment to knowledge sharing, technology transfer, and people-centred development, particularly in areas such as climate adaptation, disaster risk reduction, and sustainable development.
He also highlighted the Belt and Road Initiative as a framework that extends beyond infrastructure to include scientific cooperation, academic exchange, and innovation-driven development, with the Joint Laboratory standing as a model of how universities can advance diplomacy through science.
Makerere’s Multidisciplinary Strength at the Core
In his concluding remarks, Prof. Nawangwe reaffirmed Makerere University’s readiness to operationalize the Laboratory through a multidisciplinary research team spanning public health, geography, engineering, computing, artificial intelligence, social sciences, and the built environment.
He stressed that effective disaster management must integrate technology, human behaviour, governance, and community engagement, noting the importance of sociological insights in addressing risk perception and public compliance during disasters. Makerere will also engage emerging universities and regional partners to ensure the Laboratory’s benefits are widely shared.

The Vice-Chancellor also commissioned an interim, multidisciplinary coordination committee to operationalise the Joint Laboratory, drawing expertise from health, climate science, engineering, artificial intelligence, social sciences, and government agencies.
Hon. John Chrysostom Muyingo Officially Launches the Laboratory
The Joint Laboratory was officially launched by the Honourable John Chrysostom Muyingo, Minister of State for Higher Education, who applauded Makerere University and Tsinghua University for securing the prestigious grant and advancing Uganda’s science and research agenda.

Hon. Muyingo reaffirmed the Government’s commitment to supporting research that informs national development, public safety, and disaster preparedness. He urged Ugandan researchers to fully leverage the partnership to learn from China’s experience in transforming research into actionable solutions for society.
“This Laboratory is a clear demonstration of how strategic international partnerships can strengthen national capacity, inform policy, and protect lives,” the Minister said, as he formally declared the symposium and laboratory launch open.
Positioning Makerere as a Regional Centre of Excellence
Makerere University already plays a critical role in public safety, disaster preparedness, and early warning through a range of research, training, and operational partnerships. Through the School of Public Health (MakSPH) and the Infectious Diseases Institute (IDI), the University has led national and regional initiatives in epidemic preparedness, emergency response, and early warning, including Field Epidemiology Training, risk prediction modelling, and multi-hazard risk assessments that inform district and national preparedness planning. A national assessment of 716 health facilities conducted by MakSPH revealed widespread exposure to climate-related hazards and systemic preparedness gaps, directly informing the Ministry of Health’s Climate and Health National Adaptation Plan (H-NAP 2025–2030)
Makerere has also been at the forefront of disaster risk reduction innovation and community resilience through the Resilient Africa Network (RAN), which has supported scalable, evidence-based solutions such as EpiTent, a rapidly deployable emergency health facility; RootIO, a community-based radio communication platform used for risk communication and early warning; and RIAP Horn of Africa, which advances climate-resilient water harvesting technologies for drought-prone pastoralist communities.

Earlier, the University led the USAID-funded PeriPeri U project (2014–2019) and a disaster management collaboration with Tulane University, strengthening applied research, training, and early warning systems across Africa, efforts that laid the foundation for RAN and Makerere’s current disaster resilience agenda.
In collaboration with government and international partners, Makerere has supported the strengthening of Emergency Operations Centres, including the development of Regional Emergency Operations Centre (REOC) dashboards to improve real-time coordination and situational awareness. IDI has further contributed to epidemic intelligence and early warning, supporting districts to update WHO STAR-based risk calendars, strengthen sub-national preparedness, and enhance real-time decision-making during outbreaks. Makerere teams have also been deployed regionally to support Marburg and Mpox outbreak responses in Rwanda and the DRC, while advancing outbreak modelling as an early warning tool for high-consequence infectious diseases.
Complementing these efforts, the Department of Geography, Geo-Informatics and Climatic Sciences conducts transdisciplinary research on floods, landslides, droughts, soil erosion, and land-use change, using geospatial analysis, earth observation, modelling, and participatory methods to translate complex data into actionable early warning and risk information for policymakers and communities. These ongoing initiatives collectively demonstrate Makerere University’s established capacity in public safety, disaster preparedness, and early warning, providing a strong operational and scientific foundation for the China–Uganda Belt and Road Joint Laboratory.
With strong backing from the Governments of Uganda and China, as well as leading international partners, the China–Uganda Belt and Road Joint Laboratory on Natural Disaster Monitoring and Early Warning is poised to become a regional centre of excellence for disaster risk reduction research, training, and innovation.
The Laboratory will contribute to improved early warning systems, faster emergency response, stronger policy coordination, and enhanced scientific capacity, cementing Makerere University’s role at the forefront of addressing some of the most pressing public safety challenges facing Uganda, Africa, and the global community.
Caroline Kainomugisha is the Communications Officer, Advancement Office Makerere University.
Health
Makerere University Explores Strategic Partnership with Tsinghua University in Safety Science, Disaster Resilience and Public Health
Published
3 weeks agoon
December 16, 2025
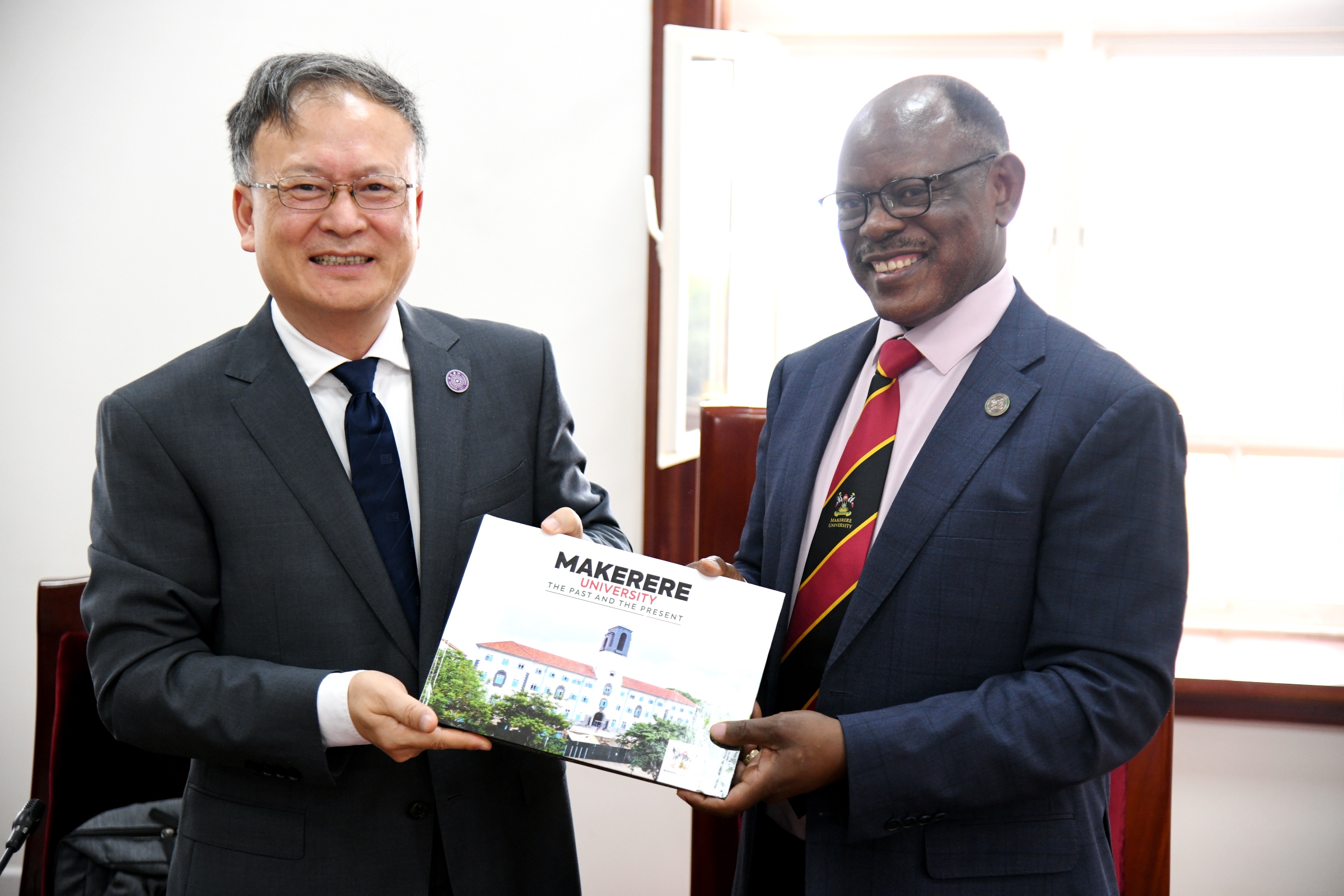
Makerere University has taken a significant step toward strengthening global research collaboration following a high-level meeting between Vice Chancellor Prof. Barnabas Nawangwe and a delegation from Tsinghua University’s Hefei Institute for Public Safety Research, one of China’s leading centres of excellence in disaster prevention, public safety, and emergency management. The engagement marked a renewed commitment to advancing scientific cooperation between the two institutions, particularly in addressing complex environmental and public health challenges that continue to shape national and global development.
A Partnership Anchored in Shared Challenges and Global Priorities
In his remarks, Prof. Nawangwe emphasized that the concept of comprehensive public safety, spanning natural disasters, epidemics, infrastructure failures, and social risks, is increasingly relevant to all colleges and disciplines at Makerere. Uganda’s experience with epidemics such as Ebola, cholera, and COVID-19; frequent landslides in mountainous regions; flooding events; and rising traffic-related incidents place the University in a unique position to contribute applied research, community-based insights, and local knowledge to a global scientific dialogue.
He noted that the Tsinghua presentation revealed new areas of alignment, particularly in epidemic modelling, early-warning systems, and integrated emergency management, areas where Makerere’s public health scientists, medical researchers, and social scientists have extensive expertise.
“This collaboration offers meaningful opportunities for nearly every college at Makerere,” he noted. “Public safety touches the environment, public health, engineering, social sciences, ICT, humanities, and urban planning. The challenges we face as a country make this partnership both timely and essential.” Prof. Barnabas Nawangwe noted.
Tsinghua University: A Global Leader in Comprehensive Public Safety.
The delegation from Tsinghua University outlined China’s national investment in Public safety over the past two decades, an effort driven by the recognition that life and security are the foundation of sustainable development. Tsinghua’s Hefei Institute for Public Safety Research has developed nationally recognised research platforms and large-scale simulation facilities dedicated to Natural disaster modelling (earthquakes, landslides, floods, typhoons, Infrastructure and urban systems safety, Public health emergencies and epidemic preparedness, Early-warning, monitoring, and emergency communication, Traffic and transportation safety, Post-disaster reconstruction and resilience planning.
Their systems currently support over 100 provincial and municipal emergency management centres in China, underscoring their global leadership in practical, scalable solutions for disaster risk management. The delegation reaffirmed that Uganda’s lived experience with multiple hazards presents opportunities for meaningful knowledge exchange. They expressed particular interest in learning from Makerere’s work on epidemic response, community health systems, and the social dimensions of disaster management.
Emerging Areas of Partnership
The meeting identified several promising pathways for long-term collaboration:
1. Joint Research in Disaster Risk Reduction and Climate-Related Hazards
Both institutions expressed readiness to co-develop research projects on landslides, floods, urban resilience, and multi-hazard modelling, drawing on Tsinghua’s advanced simulation technologies and Makerere’s environmental expertise and geographic field realities.
2. Public Health Emergency Preparedness and Epidemic Response
Makerere’s renowned public health schools and research centres will collaborate with Tsinghua on epidemic prediction, early-warning systems, and integrated preparedness frameworks, leveraging Uganda’s decades of experience managing high-risk disease outbreaks.

3. Infrastructure and Urban Safety, Including Traffic Systems
With Uganda experiencing rapid urbanisation and high rates of motorcycle-related road incidents, Tsinghua shared insights from China’s own transformation, including infrastructure redesign, transport modelling, and public transit innovations. Collaborative work in this area would support city planning and road safety interventions in Kampala and other urban centres.
4. Academic Exchange and Capacity Building
Both sides expressed interest in student exchanges, staff mobility, co-supervision of postgraduate research, and specialised training programmes hosted at Tsinghua’s world-class safety research facilities.
5. Development of a Joint Public Safety Laboratory at Makerere
The institutions are exploring the establishment of a collaborative safety research platform in Uganda. This initiative could serve as a regional hub for innovation in emergency management, environmental safety, and technology-driven risk assessment.
Towards a Long-Term, Impactful Collaboration
The meeting concluded with a shared commitment to develop a structured partnership framework in the coming months, supported by both universities and aligned with Uganda–China cooperation priorities. Both teams acknowledged that the partnership must yield tangible results that enhance community resilience, bolster national preparedness systems, and foster scientific capacity for future generations.
Prof. Nawangwe commended Tsinghua University for its willingness to co-invest in research and capacity building, noting that such collaborations position Makerere not only as a leading research institution in Africa but as an active contributor to global scientific progress.

“This partnership has the potential to transform our understanding of the science of public safety to deliver solutions that safeguard lives.” Prof. Barnabas Nawangwe noted.
“It aligns perfectly with Makerere’s mission to be a research-led, innovation-driven university responding to the world’s most urgent challenges.” He added.
As part of this strategic partnership engagement, Makerere University will, on Wednesday, 17th December, co-host the Makerere University–Tsinghua University Symposium on Public Safety and Natural Disaster Management. The symposium will run from 8:00 AM to 2:00 PM in the University Main Hall, Main Building.
This symposium represents a deepening of collaboration not only between Makerere University and Tsinghua University, but also a broader strategic partnership between Uganda and the People’s Republic of China.
During the event, H.E. Zhang Lizhong, Ambassador of the People’s Republic of China to Uganda, together with the State Minister for Higher Education, Government of Uganda, will officially launch the China–Uganda Belt and Road Joint Laboratory on Natural Disaster Monitoring and Early Warning. The Laboratory will be hosted at Makerere University, positioning the University to play a central role in strengthening Uganda’s and the region’s capacity for natural disaster preparedness, public safety, and emergency management research.
Caroline Kainomugisha is the Communications Officer, Advancement Office, Makerere University.
Trending
-

 General4 days ago
General4 days agoAdvert for the Position of the Second Deputy Vice Chancellor
-

 General5 days ago
General5 days agoUNDP and JNLC hold training in Fort Portal: Participants equipped with skills in Advocacy and Gender Equality, Team Building, Inclusive Leadership, and Financial Literacy
-

 General5 days ago
General5 days agoBreaking the Silence on Digital and Gender-Based Violence: Male Changemakers Lead Makerere University’s Strides for Change
-

 Health4 days ago
Health4 days agoMakCHS Strengthens Internationalization through Strategic Global Partnerships and Mobility
