Health
Research Links Social Support to Improved Contraceptive Decision-Making for Women
Published
10 months agoon

Researchers at Makerere University School of Public Health (MakSPH) are urging the Ugandan government to boost healthcare funding to enhance reproductive health services. Dr. Dinah Amongin, an obstetrics and gynecology expert at MakSPH, has expressed concern about the lack of access to family planning methods, which forces women to use less preferred options due to unavailability.
Dr. Amongin notes that within just six months to a year of using contraception, some women encountered issues and switched methods. This highlights the need for the Ministry of Health to improve the availability of various contraceptive options. A rights-based approach to contraception ensures that women have access to a range of methods, preventing situations where desired options are unavailable at health facilities.
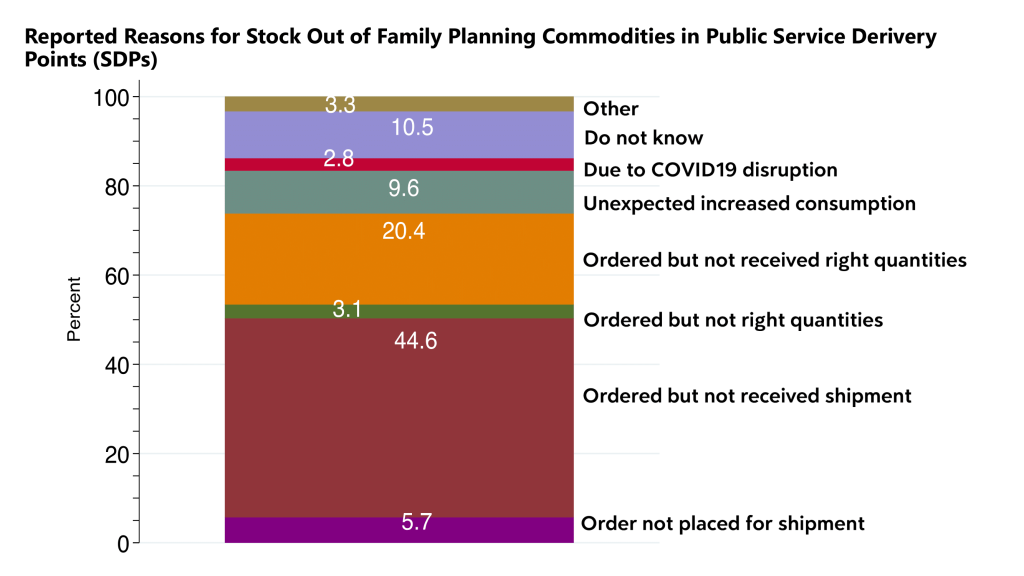
“Stockouts are a significant issue, and this extends to parliamentary discussions on health sector budgets. As we focus on human capital development and improving maternal and newborn health outcomes, we must consider crucial components like preventing unwanted pregnancies through family planning. The budget allocation for the health sector directly impacts this issue. When women cannot access their preferred contraceptive methods due to stockouts, it reflects a failure in our legislative and budgeting processes. This situation forces women to switch to fewer desirable methods, which is not acceptable,” says Dr. Amongin.
Adding that; “These are things we need to continue discussing as a country but we must invest into family planning. We can talk about human capital development but until we step up and actually support women to prevent unwanted pregnancies, support them in their decisions of whether she wants to use a method for contraception or not. That is her choice. We must make sure access to the methods of her choice is actually addressed.”

Dr. Amongin’s comments follow a recent study on the I-CAN/Nsobola/An atwero social support intervention, piloted in Mayuge and Oyam districts in 2023. The study highlights that social support significantly improves women’s ability to make informed contraceptive choices, potentially leading to better reproductive health outcomes.
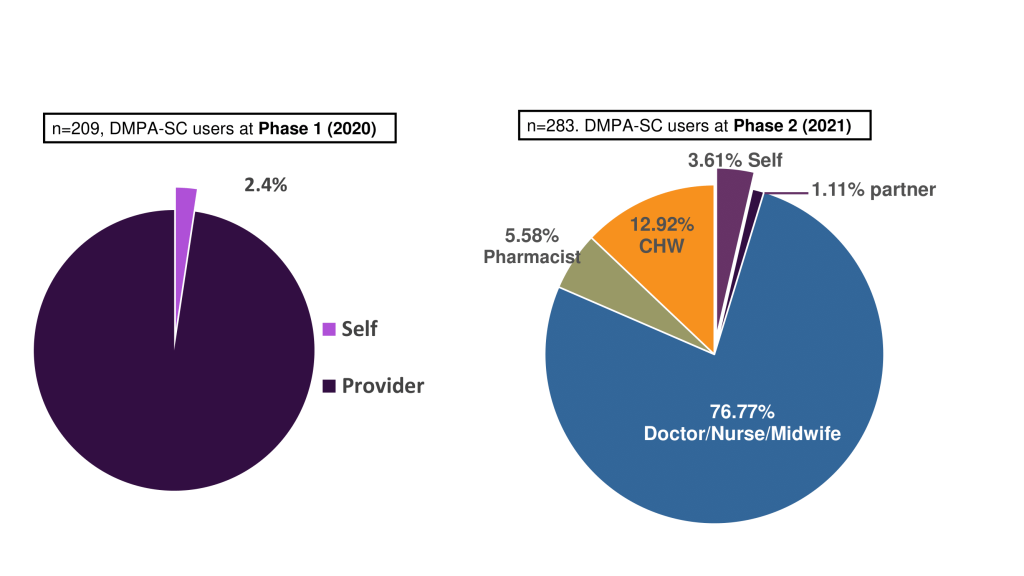
Part of the Innovations for Choice and Autonomy (ICAN) project, the study shows that self-injection with DMPA-SC (Sayana Press) could increase contraceptive use, especially among women with limited access to healthcare. Despite the rollout of this method in 2017, its use remains low in Uganda. Sayana Press as popularly known is a subcutaneous depot medroxyprogesterone acetate (DMPA-SC). It is a hormonal birth control shot, administered under the skin and is an all-in-one contraceptive that puts women in charge of their reproductive health.
Social support boosts self-efficacy, enhances privacy, and reduces access barriers, making self-management easier. Family planning helps manage the number and timing of children, lowering maternal and infant mortality rates and reducing complications from pregnancy. Conversely, unmet contraceptive needs can lead to unintended pregnancies and their associated risks.

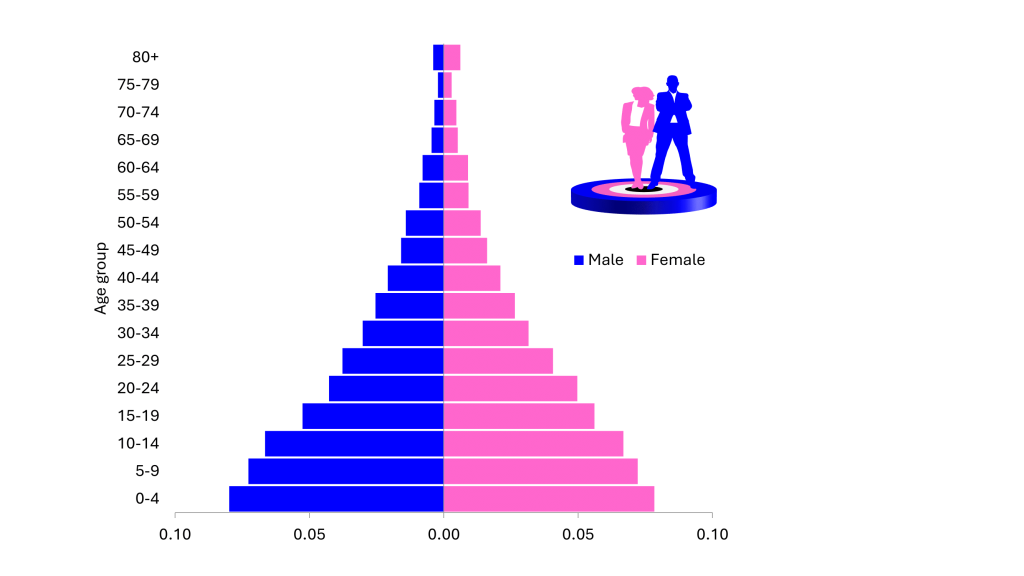
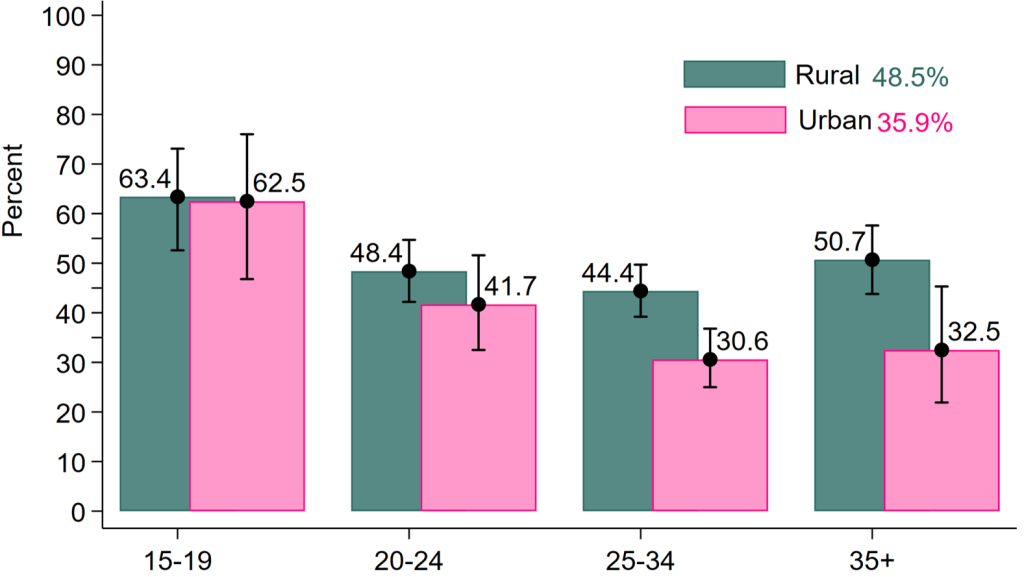
In Uganda, 52% of pregnancies are unwanted or mistimed, with over 43% due to unmet family planning needs. The country’s youthful population complicates the issue, with 50% under 17 years old, at least according to the recent National Population Census. Notably, 10% of girls, one in every 10 girls you encounter, has already had sex before she turns 15 years, and 20% of boys, two in 10 boys have engaged in sexual intercourse by the same age.
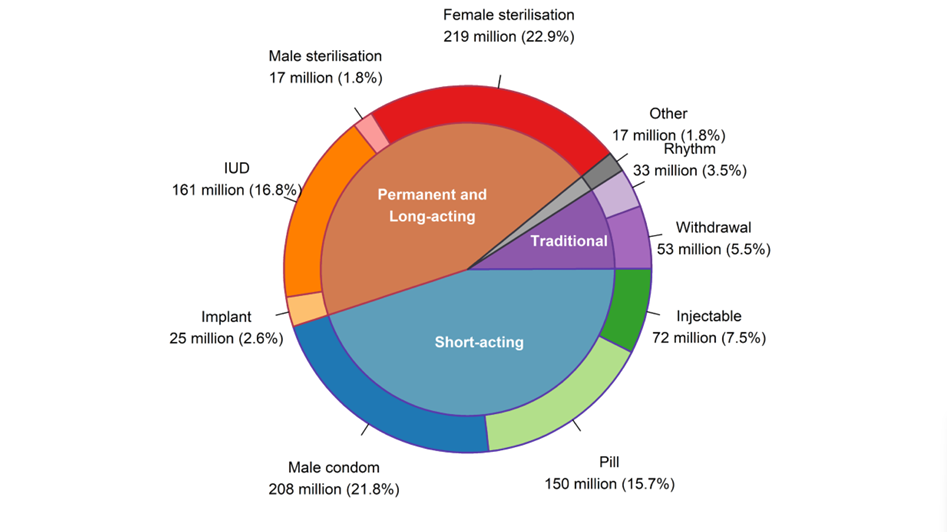
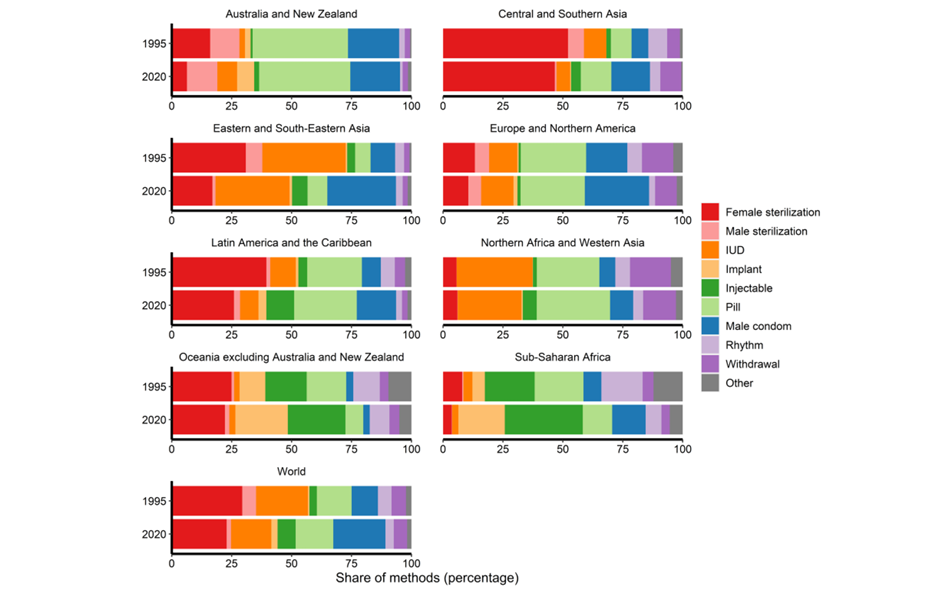
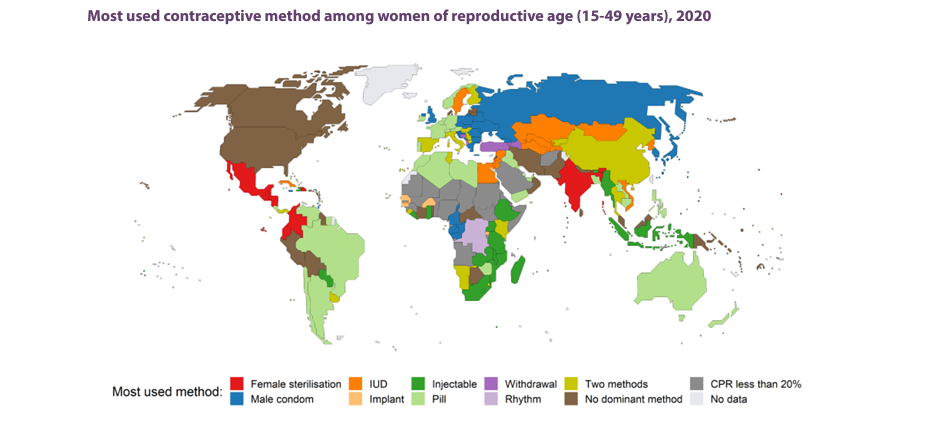
Methods of contraception include oral contraceptive pills, implants, injectables, patches, vaginal rings, intra uterine devices, condoms, male and female sterilization, lactational amenorrhea methods, withdrawal and fertility awareness-based methods.
Global statistics show that 77.5% of women aged 15–49 had their family planning needs met with modern methods in 2022, up from 67% in 1990. In sub-Saharan Africa, the proportion of women who have their need for family planning satisfied with modern methods (SDG indicator 3.7.1) continues to be among the lowest in the world at 56 per cent. Nevertheless, it also increased faster than in any other region of the world, having more than doubled since 1990, when this proportion was only 24 per cent.
Among 1.9 billion women of reproductive age (15-49 years), an estimated 874 million women use a modern contraceptive method and 92 million, a traditional contraceptive method. The number of modern contraceptive users has nearly doubled worldwide since 1990 (from 467 million). Yet, there are still 164 million women who want to delay or avoid pregnancy and are not using any contraceptive method, and thus are considered to have an unmet need for family planning.
Slow progress is due to factors like limited method choices, restricted access, fear of side effects, cultural opposition, and gender-based barriers.
Between 2015 and 2019, there were 121 million unintended pregnancies annually worldwide – 48 per cent of all pregnancies. Despite decreases in the rate of unintended pregnancy in all regions over the past three decades, nearly one in 10 women in sub-Saharan Africa, Western Asia and Northern Africa, and Oceania (excluding Australia and New Zealand) continue to experience an unintended pregnancy every year
In Uganda, where healthcare services are stretched thin and women juggle numerous responsibilities, accessing contraceptives can be challenging.
Dr. Amongin emphasizes that self-injection methods like DMPA-SC, also known as Sayana Press could ease the burden on women facing long queues and logistical challenges at health facilities. “This method allows for discretion and reduces the need for frequent visits, which is crucial for women with busy lives,” she says.
Researchers argue that the health sector’s budget should include substantial funding for family planning. The high cost of inaction is evident: neglecting family planning leads to unplanned pregnancies, which ultimately burdens families and the nation. Addressing this issue early in the life cycle is crucial to prevent these long-term consequences.
“This is the gist of the matter behind all our research, that a woman’s preference needs to be respected. The health facilities must stock commodities so that when a woman is in need, she actually gets it,” noted Dr. Amongin.
Dr. Peter Waiswa, an Associate Professor at MakSPH, stresses the importance of informed choice in family planning. ICAN studies across Kenya, Malawi, Nigeria, and Uganda show that self-injection benefits all women, including young adolescents. “Supporting young people to make informed choices helps prevent unintended pregnancies,” says Prof. Waiswa.
“We spent four years trying to understand which women benefit from injecting themselves. And we found that all women benefit from it, including younger children. Because younger children in Uganda, whether we hide our heads in the sand or not, especially those 12 years and above are having sex and some of them using contraceptives,” Professor Waiswa says.

What is factually true is that by age 18, 60% of Ugandans have reported having sexual intercourse. Despite the benefits, dropout rates from family planning methods remain high due to side effects and lack of support. Dr. Waiswa also, a Public Health specialist, critique and dreamer for better health systems for mothers, newborns and children in Africa calls for better education and support to address these issues.
“As a way of being supported in a safe space whereby people are not asking questions, they are not fearing parents, they are not fearing other people, then they can use the methods. What we did in Mayuge and Oyam, we trained women who are users of family planning. To identify people who need to use family planning but are not currently using and then they go and see whether they can use or not. And we found that when people are supported, those groups which are currently not being reached can be reached by family planning,” argues Prof. Waiswa.
A 2021 study found that contraceptive discontinuation significantly impacts the effectiveness of family planning services, leading to higher fertility rates, unwanted pregnancies, and induced abortions.
Analysis of data from PMA 2020 show that 6.8% of women discontinued contraceptive use, with discontinuation linked to factors such as age, marital status, method type, and health concerns. The study suggests prioritizing interventions to encourage contraceptive use among young people and promoting partner involvement and awareness, as many contraceptive methods are not discreet.
Prof. Waiswa is concerned of the high dropout rate from family planning methods, where many women discontinue use due to side effects, a need for better education and support.
“We need to see how to educate women so that they are informed when they are choosing a method to use. They need to have enough information because when they discontinue, the method can be ineffective, can cause side effects, but also these methods are expensive, so they waste money. There are a lot of those who change to other methods. We are learning a lot on the use of family planning why we still have a large unmet need,” says Prof. Waiswa.
Ms. Roseline Achola, Technical Specialist for Sexual and Reproductive Health and Self-Care at the Ministry of Health, hailed the MakSPH study on self-injection contraception. She noted that the findings will help her enhance support for self-care initiatives. However, she expressed that only 29% of women willing to self-inject as indicated in the study is still low, highlighting a need to address barriers to increase acceptance as well as managing sexually active adolecents. “We must discuss how to handle minors seeking contraception to prevent unintended pregnancies,” she says.
On Friday August 23, 2024, the Daily Monitor reported, an increase in young girls adopting family planning to combat teenage pregnancies and school dropouts. Quoting data from the Uganda Health Information System, statistics show that between March 2023 and March 2024, 2,476 girls under 15 had their first antenatal care visit, and 1,755 gave birth. The highest number of pregnancies among this age group was in Oyam district.
In this period, Lango subregion saw 52 pregnancies among this age group, with Oyam district recording the highest at 10 cases. The 2021 UNFPA fact sheet indicates that Busoga region, particularly Kamuli and Mayuge districts, has the highest rates of teenage pregnancies, with 6,535 and 6,205 cases respectively.
“As the country, it’s clear that adolescents are limited to access to contraception because of so many reasons. For us as a Ministry, any woman between the age of 15 to 49 is a woman of reproductive age and that tells you that she is capable of getting pregnant and when such a girl of probably 15 years goes to a facility to seek for contraception, it rings a message that actually she is sexually active. So how do we handle her? So that is a matter of discussion for the country.
It is a matter that the nation needs to decide on, because we all know the girls are getting pregnant, the girls want to use contraception, but they have no access because of the fact that they are children,” wondered Achola.

Unintended pregnancies and Uganda’s abortion paradox
Abortion in Uganda, is largely illegal except in specific circumstances. It contributes to maternal death due to unsafe practices. Between 2010 and 2014, WHO reported that 30.6million abortions conducted were safe and 25.1million were unsafe. 97% of these occurred in developing countries. In East Africa, the total number of abortions per year according to the Lancet are around 2.65million.
The Ministry of Health’s HMIS data show a rise in abortion cases, with 96,620 reported between July 2020 and June 2021in both government and private health facilities.
Another recent study on the quality of post-abortion care by MakSPH researchers Assoc. Prof. Lynn Atuyambe, Dr. Justine Bukenya, Dr. Arthur Bagonza and Mr. Sam Etajak highlights the need for accurate post-abortion care data to improve healthcare planning and policymaking.
Dr. Arthur Bagonza, a Public Health Consultant and Research fellow with specialization in health systems at MakSPH and one of the uality of post-abortion care has called for accurate abortion data to improve healthcare planning and policymaking. He notes that health workers often avoid documenting abortion data due to legal fears and calls for reforms to restrictive laws to ensure accurate reporting without legal repercussions.
“All assessed health facilities reviewed in our study achieved a 100% timeliness rate for report submissions. However, significant disparities were observed in data accuracy between different levels of health facilities, with lower-level facilities (HC IIs and HC IIIs) showing higher rates of data discrepancies,” says Dr. Bagonza.

According to Dr. Amongin, the high incidence of early sexual activity among Uganda’s youth is a pressing public health issue.
“We know as a country many women continue to die following unsafe abortions; abortions for pregnancies that they did not want. And these abortions are highest among adolescents and also other women categories.
We would want to ensure that we actually enhance access to contraceptives, but making it easier for them to have it and putting the power in the hands of a woman to as much extent as we can. So that a woman can practice what we call self-care, but of course she also will need the support of the healthcare system. But we want this power in women’s hands because of all the challenges that the women actually can encounter in accessing these methods,” she said.
On her part, Achola insists that abortion should not be a last resort for women and urges them to abstain or use protective means in order to avoid unwanted pregnancies. She notes that as long as abortion remains illegal in Uganda, many health workers will avoid addressing it, leading people to unsafe alternatives.
“I can’t be happy because abortion means we have failed to give people a method of their choice to prevent that pregnancy. Or the people are not able to access contraception to prevent unintended pregnancies. Abortion is not the last resort, it’s not a solution because it has its own complications as well,” says Achola.

Despite this, Achola, notes most of the women who walk in health facilities with post-abortion complications must be attended to. “Whereas we don’t encourage people to do abortions, as Ministry of Health we are mandated to handle all complications for anyone who walks in our facilities because our priority is to save life. We want to urge women to avoid certain things. Why should you wait for unintended pregnancy to occur and then abort?”
Dr. Charles Olaro, a Senior Consultant Surgeon and the Director Health services – Curative in the Ministry of Health highlights the financial burden on individuals seeking health services and suggests exploring private sector opportunities and community-based approaches to improve access. “We need to balance values and rights while addressing access barriers,” he notes.
According to Dr. Olaro, the autonomy and agency of women in sexual and reproductive health, particularly in African cultures remain a challenge where social norms may require women to defer decisions to their partners.

He notes that there is a high burden of abortion and self-harm, with a significant portion of maternal mortality attributed to sepsis, which is often a result of unsafe abortions in Uganda.
“We still need evidence to ensure that access barriers are addressed. And this is a question I keep on asking Makerere University, yes, we have a young population but how are these people accessing contraceptives. Other issue we have to deal with is complex. I know we have to do a balance between values and rights, but we will be able to look at that when they gain the success to do it.”
Dr. Olaro points out that individuals often face a financial burden in health services, spending more on prescriptions than on the medications themselves. He suggests exploring private sector opportunities and a community-based approach to improve access to healthcare.
NB: The PMA surveys are spearheaded by Associate Professor Fredrick Makumbi and Dr. Simon Kibira of MakSPH, with support from the Uganda Bureau of Statistics and the Ministry of Health. The initiative also receives funding from the Bill & Melinda Gates Foundation, The Children’s Investment Fund Foundation (CIFF), and is supported by the Bill & Melinda Gates Institute for Population and Reproductive Health at Johns Hopkins University and Jhpiego.
You may like
-


Emorimor Calls for Makerere to Upgrade Parenting Course
-


Uganda Deepens Economic Governance with Training on Regulatory Cost-Benefit Analysis
-


UVCF Makes Case for HEAC Programme
-


Mastercard Foundation Board pays its inaugural visit to Makerere University
-


Mak CEES discusses partnership with King Salman Global Academy for the Arabic Language
-


Meet Safali Libia, a Mastercard Foundation Scholar-alumnus who rebuilt his life as a refugee in Uganda
Health
Emorimor Calls for Makerere to Upgrade Parenting Course
Published
8 hours agoon
June 30, 2025By
Zaam Ssali
The Iteso Cultural Leader, His Highness Emorimor Papa Paul Sande Emolot, has called on Makerere University to elevate the Science of Designing, Adaptation, and Implementation of Evidence-Based Parenting Interventions course into a fully-fledged programme. This, he argued, would strengthen the capacity of practitioners implementing parenting interventions across Uganda.
Speaking at a graduation ceremony held on 11th June 2025 at Makerere University where 35 practitioners completed the 12-week course, Emorimor Papa Emolot emphasized the transformative power of effective parenting. He urged aspiring parents and advocates of the Parenting for Respectability model to enroll in the course.

Citing the impact in his own sub-county and village, the cultural leader revealed that over 800 families had already benefited from the programme.
“We now see peace and love in homes where there was once conflict. Without good parenting, you risk raising animals instead of children,” he passionately stated.
He praised the course for equipping practitioners, policymakers, and researchers with the skills needed to design culturally sensitive, evidence-based parenting interventions tailored to Uganda’s context. Among the notable graduates was Her Royal Majesty Juliet Among Emolot Atomeileng Akaliat Toto, who reaffirmed her commitment to advancing family-strengthening initiatives using the skills and knowledge acquired.

Dr. Godfrey Siu, Senior Lecturer and Course Leader at Makerere University, described the course as a timely intervention. During this remarks, Dr. Siu described the event as a significant milestone in advancing the field of evidence based parenting intervention and family strengthening in Uganda.
“This course is meant to empower you as practitioners, policy makers and all those involved in development and implementation of parenting work. It provides both theoretical knowledge and practical tools essential for developing high quality interventions”, Dr. Siu noted. He urged the pioneer group to carry forward the expertise as champions of designing, adaptation and implementation of evidence parenting interventions.

Representing the Permanent Secretary of the Ministry of Gender, Labour and Social Development, Dr. Aggrey David Kibenge, Juliana Naumo, Commissioner for Culture and Family Affairs, said the course supports the government’s agenda to address negative social outcomes affecting families.
“By grounding parenting in research, harmonizing policy with practice, and advocating for equity, we will ensure no family is left behind,” she said. “Cross-sectoral collaboration is key to unlocking transformative change.”

Ms. Naumo highlighted the government’s commitment—both technical and financial—to support outstanding student projects from the course. She stressed the importance of equipping professionals with the skills to bridge gaps between research and practice for consistent, high-quality parenting support across Uganda. While delivering the Vice chancellors speech by Dr. Helen Nambalirwa, Principal of the CHUSS, Prof. Barnabas Nawangwe commended the graduates as a beacon of hope.
“At a time when parenting faces challenges like digital distractions, changing societal norms, and a rising mental health crisis, Makerere reaffirms its support for interventions that drive the societal transformation we desire,” Nawangwe stated.
Prof. Richard Idro, Deputy Principal of the College of Health Sciences, acknowledged the growing parenting challenges in Uganda and the region, adding that the course was a major step towards standardizing parenting interventions nationwide.

He applauded the Child Health and Development Centre (CHDC) for leading this paramount and critical initiative.
Mr. Hosea Katende, Course Administrator at CHDC, emphasized the importance of integrating systematic methods, ethical principles, robust evidence, and collaboration to create lasting impact in parenting.

Dr. Aggrey Dhabangi, Lecturer at CHDC, representing Dr. Herbert Muyinda, Director of CHDC, acknowledged the contributions of partners such as the ELMA Foundation and Echidna Giving for their financial and capacity-building support. He also appreciated the Ministry of Gender, Labour and Social Development, among other stakeholders, for their technical guidance in the programme’s successful implementation.
Dr. Dhabangi extended gratitude to cultural institutions, especially the Kingdom of Teso, and acknowledged growing collaborations with other cultural institutions such as the Kingdom of Acholi, in the shared mission of building strong families as the foundation of Uganda’s future.

He extended his heartfelt gratitude to cultural institutions, especially the Kingdom of Teso, and others kingdoms such as the Kingdom of Acholi, in building Uganda’s future through creating strong families. Nuruh Mbalyowere, a Rehabilitation and Reintegration Officer with the Uganda Prisons Service, was honored for developing the best parenting intervention titled “Parenting Behind Prison Bars.” She expressed her intention to apply the knowledge gained both at home and in her workplace.
Health
MakSPH, DJC Launch Short Course on Health Communication
Published
1 week agoon
June 20, 2025
By Okeya John and Primrose Nabankema
The intensive one-month course, running for the first time from June 5 to July 24, 2025, is jointly offered by Makerere University School of Public Health (MakSPH)’s Department of Community Health and Behavioural Sciences (CHBS) and the Department of Journalism and Communication (DJC) at the School of Languages, Literature, and Communication (SLLC), co-designed in 2024 with support from the Rockefeller Foundation through Amref Health Africa.
It seeks to equip healthcare providers at the community level, public health and environmental health practitioners, communication specialists, health educators, community development officers, social scientists, and policy makers, among others, with strategic communication skills to improve public health messaging, strengthen community engagement, and support evidence-based interventions, ultimately empowering participants to effectively engage communities and improve population health outcomes across Uganda and the region.
Launching the course, the heads of the Department of Journalism and Communication and the Department of Community Health and Behavioural Sciences noted that participants who complete the short course will gain practical tools to influence behaviour change, build trust, and deliver timely, accurate, and relevant health information to the communities they serve. The first cohort attracted more than 60 applicants, with 36 reporting for the opening in-person session on June 5, 2025, at MakSPH in Mulago. Between now and July, participants will undergo a hands-on, multidisciplinary learning experience within the Certificate in Health Communication and Community Engagement program, which combines theory and practice.
Among the participants in the first cohort of the certificate course, designed as a pilot for the anticipated Master of Health Promotion and Communication to be jointly offered by the two departments at Makerere University, is Ms. Maureen Kisaakye, a medical laboratory technologist specialising in microbiology and antimicrobial resistance (AMR), and currently pursuing a Master’s in Immunology and Clinical Microbiology at Makerere. She is driven by a passion to help reverse the rising tide of AMR, a growing global health threat where drugs that once worked are no longer effective. Kisaakye is particularly concerned about common infections, like urinary tract infections, becoming increasingly resistant and harder to treat.
“I enrolled in this course because I’m an advocate against antimicrobial resistance, and it came at a time when I needed to deepen my knowledge on how to implement our projects more effectively and engage with communities. The experience has broadened my understanding of AMR and its impact on society, and strengthened my passion for community-driven health initiatives and advocacy,” Kisaakye said, explaining why she enrolled for the short course.

Kisaakye’s work in antimicrobial resistance extends beyond the lab. Having earned her degree in medical laboratory science from Mbarara University of Science and Technology, she founded Impala Tech Research in 2024 to drive impact and save lives. She has led grassroots AMR campaigns that integrate antimicrobial stewardship with water, sanitation, and hygiene (WASH) education in underserved urban communities, including the informal settlements in Kampala. She also has since designed peer-led initiatives that empower university students as AMR Champions, building a network of informed youth advocates. Kisaakye believes the health communication course will sharpen her ability to design and deliver impactful, community-centred interventions in response to the growing threat of drug resistance.
“The department collaborates with many partners within and beyond the University, including the School of Public Health, where we are working to develop the subfield of health communication and promotion. Our goal is to train specialists in this area and build a community of practice, something we have each been doing in our own spaces. There’s a lot of work ahead, and COVID-19 showed us just how urgently we need a generation trained to do this kind of work, and to do it very well,” said Dr. Aisha Nakiwala, Head of the Department of Journalism and Communication, during the opening of the short course on June 5.

She assured participants they were in good hands and underscored the importance of the partnership between the Department of Journalism and Communication and the School of Public Health, describing it as a vital collaboration that brings together strategic communication and public health expertise. This dynamic, multidisciplinary approach, she noted, is essential to developing practical solutions that empower communities, strengthen health systems, and ultimately improve livelihoods.
The course offers a hands-on, multidisciplinary learning experience, with participants intended to explore key modules including Health Communication and Promotion, Risk Communication, Smart Advocacy, Community Mapping, Community Mobilisation and Empowerment, and Strategies for Community Engagement. The course combines theory with real-world application, and its assessment includes a field-based project and a final exam.
“You are our first cohort. We are seeing the fruits of our efforts in bringing this short course to life. It was born out of a joint initiative to develop a Master’s programme in Health Promotion and Communication,” said Dr. Christine Nalwadda, Head of the Department of Community Health and Behavioural Sciences. “We carried out extensive consultations with our different key stakeholders during the process and discovered a real need for such a course. It was the stakeholders who even named it; this course name didn’t come from us.”
For Kisaakye, by the end of the course in July, she hopes to have sharpened her skills in health promotion and strategic communication, particularly in crafting targeted messages that help individuals and communities effectively respond to threats such as antimicrobial resistance. She also aims to gain practical experience in designing, implementing, and evaluating community health initiatives that can strengthen her advocacy and drive lasting impact.

Health
Call for Abstracts: 2nd East African Symposium and Expo on Trauma, Injuries, and Emergency Care – 2025
Published
2 weeks agoon
June 19, 2025By
Mak Editor
The Makerere University School of Public Health (MakSPH) is excited to invite researchers, professionals, and students to be part of an inspiring and impactful event!
Venue: School of Public Health Auditorium, Makerere University Main Campus
Dates: August 7–8, 2025
Theme: “Understanding the burden and impact of injuries in East Africa to improve Emergency Care preparedness, mitigation, and response.”
Submit Your Abstracts Now!
Join the conversation that drives change in trauma and emergency care across East Africa. Share your research, innovations, and insights that can shape the future of healthcare response in our region.
Submission Deadline: July 10, 2025
Submit here: triadcommunications@musph.ac.ug
Register to Attend: https://aapug.org/east-african-symposium-and-expo-on-trauma-injury-disability-and-emergency-care-2025/
Together, let’s drive change and improve lives through research and collaboration. Don’t miss this opportunity to make a difference!
Trending
-

 General3 days ago
General3 days agoMature Age Scheme Exam Results for 2025/2026
-

 General6 days ago
General6 days agoFreshers’ Joining Instructions 2025/2026
-

 General1 week ago
General1 week agoMastercard Foundation Board pays its inaugural visit to Makerere University
-

 General1 week ago
General1 week agoUVCF Makes Case for HEAC Programme
-

 Natural Sciences2 weeks ago
Natural Sciences2 weeks agoCoNAS Participates in the 2025 National Science Week Exhibition
