Health
Former Grade III Teacher graduates with a PhD: NCDC approves her Study Intervention for Adolescent Care
Published
2 years agoon

Sixty four-year-old Sarah Bunoti Nantono is a retired teacher and Lecturer of Psychology. She enrolled for a Ph.D. program at Makerere University School of Public Health (MakSPH) in 2013 with the goal of studying early adolescent reproductive health.
Having taught for more than thirty years, Dr. Sarah Bunoti Nantono had moved up the academic ladder from being a primary school teacher to a lecturer at Kyambogo University. She believed that earning a PhD would be her ultimate goal in life. While at Kyambogo University, the second largest of the now 13 public universities in Uganda, Dr. Sarah Bunoti devoted her professional life to training social scientists, teachers and teacher educators.
Eleven years later, Dr. Bunoti Sarah Nantono is one of the 46 females of the 132 PhD graduands in the #Mak74thGrad, which begins on Monday, January 29, 2024.
She successfully earns a Doctor of Philosophy ( PhD) in Public Health from Makerere University following her in-depth research titled; “Pubertal and Child Rights Awareness, Communication, and Child Protection against Sexual Abuse and Exploitation among 10–14-year-olds in Jinja Primary Schools: Opportunities, Challenges, and the Effectiveness of a School-Based Intervention.”
Dr. Sarah Bunoti is a seasoned lecturer with a proven track record in teacher training, social sciences, and psychology. Holding an MSc in Environment from Makerere University Institute of Environment, she also earned a Bachelor of Science in Zoology and Psychology from Makerere University in 1999, a Diploma in Teacher Education from ITEK in 1995, and a Grade III Primary School Teachers’ Certificate from the National Institute of Education. Beginning her career in 1981 as a primary school teacher, and later as a Teacher Trainer in the Ministry of Education in 1995, Sarah transitioned to Kyambogo University in 2000, where she currently serves as a part-time Lecturer, following her retirement. Sarah Bunoti Nantono is not only an educator but also an accomplished author, contributing to the development of the Child Rights Curriculum (CRED-PRO).
Dr. Sarah Bunoti’s PhD research examined how Jinja primary school children, aged 10 to 14, understood puberty and their rights related to sexual and reproductive health (SRH). The study looked at their knowledge sources, difficulties, and prospects for managing pubertal health effectively.
The 10-14 age group comprises 10% of the global population, with Uganda having a higher percentage at 16%. This period marks the onset of significant changes, known as the storm in Psychology, involving body transformations and social shifts.
According to Dr. Sarah Bunoti, timely support during these changes fosters a sense of achievement, but delays can lead to anxiety and unpreparedness. Uganda, aligning with international agreements, including the UN Convention on the Rights of the Child, works to uphold children’s sexual well-being through policies and partnerships.
Dr. Sarah Bunoti further notes in her research that the 10-14 age group in Uganda encounters puberty during primary school without appropriate information, support, protection, or preparation for the changes, leading to psychological challenges, sexual abuse, early marriages, unplanned pregnancies, and a rise in school dropouts.
![Dr. Sarah Bunoti's PhD Defense Panel [Professor Stella Neema, Associate Professor Joseph Ssenyonga, Dr. Siu E. Godfrey, Dr. Beyeza-Kashesya Jolly and supervisors Associate Professor Lynn Atuyambe, Prof. Nazarius Mbona Tumwesigye alongside the session chairperson Prof. Garimoi Orach] determining the verdict before she was declared to have passed her defense. Davies Lecture Theatre, College of Health Sciences, Makerere University, Kampala Uganda, East Africa.](https://news.mak.ac.ug/wp-content/uploads/2024/01/Makerere-CHS-SPH-74th-Graduation-Dr-Sarah-Bunoti-Jan2024-PhD-Defense-Panel-1024x683.jpg)
Busoga region, where the study was conducted faces particularly high rates of teenage pregnancies (7%) and school dropouts (91%). Children hold misconceptions driven by myths about puberty, emphasizing the lack of systematic guidance. Current Adolescent Sexual Reproductive Health programs focus on older children in secondary schools, neglecting the needs of those under 15.
Traditional sources, like family discussions, have diminished, placing the responsibility on schools, which often lack the necessary resources and teacher training. As a result, many 10-14-year olds are ill-prepared for changes and lack protection against sexual abuse, highlighting the necessity for evidence-based school interventions to address this information gap.
“Previously in our African traditional setting, the Aunties, Uncles and grandparents talked about puberty and prepared children for adulthood however with the breakdown of African traditional settings, schools are expected to do the role of talking to children about puberty.
Unfortunately, schools often look at puberty as an issue that is concerned with the family and expect the family to do that but also one possible problem is that the teachers themselves don’t know what to do when they are preparing these children for that,” observes Dr. Sarah Bunoti.
Unfortunately, some stakeholders use threatening language, warnings, and punishments, contributing to risk behaviors, including sexual abuse, mood swings, and trauma among children.
“We wanted to find out what these children know about puberty, challenges they face and the support they get. We also wanted to find out from key duty bearers, these are parents and teachers, what kind of support do they give to the children and to what extent do they fulfill their obligations to protect the children against sexual abuse,” said Dr. Sarah Bunoti.
The study covered 16 primary schools purposefully selected for their diverse characteristics, including boarding status, religious affiliations, gender specifications, and geographical locations. The investigators also engaged with government officials to understand their stance on current sexual and reproductive health issues among young adolescents.
The study exposed deficiencies in children’s understanding of puberty and child rights, along with teachers’ inadequate knowledge and skills in teaching puberty.
Findings for instance revealed that kids—particularly boys—don’t often get the chance to talk candidly about puberty with adults. In all focus group conversations, the study gave boys and girls a forum to openly address their experiences, difficulties, and rights related to sexual and reproductive health. This emphasizes how important it is for all people to become widely sensitive to the issues that face kids. Stepmothers were found not to communicate about puberty because of generalization and others.

“Surprisingly, discussions on pubertal challenges elicited more extensive responses from both boys and girls compared to other topics. Boys, although engaging in perceived anti-social behavior, demonstrated a level of conscience. It became evident that children, despite being sexually and biologically mature, require guidance on navigating the impact of hormones on their sexual feelings. The blame for communication gaps often falls on parents, who may be absent due to work, divorce, or being orphaned,” says Dr. Bunoti.
Subsequently, she developed, applied, and assessed two intervention books; A children’s Resource book and a Teachers’ guide. The Randomized Control Trial demonstrated improved pubertal knowledge among children and enhanced teaching capabilities in teachers, affirming the intervention’s effectiveness. These intervention books were approved by the National Curriculum Development Centre (NCDC) and approved for teaching pubertal health and safety in primary schools nationwide.
Dr. Bunoti has recommended empowering and involving young communicators to convey Sexual and Reproductive Health and Rights (SRHR) information to 10-14-year-olds, working collaboratively with parents and teachers, a strategy she believes will narrow the generation gap and enhance effective communication. Additionally, she calls for increased awareness and participation of male parents and teachers in SRH communication and child protection.
“Parents and adults should supplement school-based SRHR education by instilling age-appropriate individual, family, and community values and skills rooted in social, cultural, and religious contexts. Provide specialized training for Senior Women Teachers and Male Teachers, and reduce their teaching load to ensure dedicated attention to this critical aspect of education,” Dr. Bunoti expertly says.
Her study, funded by Sida and supervised by Dr. Lynn Atuyambe and Prof. Nazarius Mbona Tumwesigye, successfully attained this recognition.
During her PhD defense, Associate Professor Lynn Atuyambe remarked, “It was a very enjoyable defense. You truly and successfully defended your PhD—now, you own your PhD.”
“I want to thank most especially your family, they’ve been part of this journey I am not guessing, I know they’ve been and am excited to see them and I like the support they have offered to mum. The highest level of education in the world is a PhD, you can do no more than that. You have reached at the saddle of your life in academia, congratulations and I wish you good luck,” said Dr. Lynn Atuyambe.
How her PhD Journey started
About a decade ago, SIDA had been consistently supporting Makerere University. However, they decided to extend their support to other public universities. When the opportunity arose, she seized it.
“I have a habit of greeting, and my children often question why I greet so much. Sometimes, it turns out to be quite beneficial. One day, I walked into my Dean Dr. J Katigo – Kaheeru’s office and greeted, asking how he was. He said, ‘Sarah, I am glad you’ve come, read this but I said Doctor I am not ready for this, but he said, ‘Sarah, you can’t give any more excuses, this is a God given opportunity, they want a concept for the SIDA Scholarships, go ahead and write a concept.’ I later met Professor Mary N Okwakol, my undergraduate Lecturer of Zoology, and Professor Albert Lutalo Bbosa, the former Vice Chancellor of Kyambogo University, who too reassured me of my potential to attain a PhD. Out of 26 submissions from Kyambogo University, only three concepts were selected, and fortunately, mine was one of them,” Dr. Sarah Bunoti recalls.
Once her concept was ready, Dr. Bunoti came to Makerere University, but her research topic was broad. Unfortunately, her background did not align with the faculties that typically received sponsorship from SIDA. Zoology, Psychology, Education, and Environmental Studies were her strengths, but none fell within the supported areas.
Feeling disconsolate, she sought guidance from the then Director of Research and Graduate Studies at Makerere University, Professor Elly Katunguka. “He said, ‘why should you really struggle looking for a home, go and try School of Public Health. With your background, you’ll find a home,” she recalls.
Acting on his advice, Dr. Sarah Bunoti visited the School of Public Health one morning. However, the Dean, Prof. William Bazeyo, then, was away on leave; “I spoke with Assoc. Prof. Fred Wabwire-Mangen, the Acting Dean at the time. I explained my situation, highlighting my expertise in teaching, psychology, and environmental studies. He encouraged me to submit my concept, assuring me that these areas were valued in public health. This led to provisional admission, and I began refining my proposal with their guidance.”
As she exited Dr. Mangeni’s office, he promptly contacted Professor Anne Katahoire, who was by then the Director of Makerere University Child Health and Development Centre and Prof. Atuyambe, who was in Nairobi for a conference and told them; “We have a prospective student here, are you willing to take her up and without hesitation, Prof. Anne said yes and Prof. Lynn said, ‘I am in Nairobi but when I come back, I want to see that student,” Sarah recollects.
Subsequently, Prof. Mangeni reached out to Prof. Nazarius Mbona Tumwesigye upon recognizing the importance of the statistics component, he promptly invited her to discuss further details at the school. “In a short span, I found myself with a dedicated team of supervisors, a supportive Doctoral Committee chaired by Prof. Christopher Garimoi Orach with Prof Joseph Oonyu (RIP) and Dr. Christine K. Nalwadda, and a scholarly home in the Department of Community and Behavioral Sciences at the Makerere University School of Public Health,” Sarah Bunoti says.
Dr. Sarah Bunoti expresses gratitude to the MakSPH PhD Forum, the MakSPH family, the funder and her mother institution -Kyambogo University for the immeasurable support.

Dr. Sarah Bunoti expresses gratitude to the MakSPH PhD Forum, the MakSPH family, the funder and her mother institution -Kyambogo University for the inestimable support. She is also grateful to head teachers, teachers, children, and parents from her 16 project schools; Jinja City and District Education, Health and Community Development officers as well as the Family and Child Protection Unit of the Uganda Police Force and others for the information and support rendered to her.
“I can’t quantify the support I received from MakSPH, from PhD forum, from my supervisors you all did a good job to support me in this. In addition, SIDA did a good job because with our teaching salary, paying for my PhD would have been a problem but they paid all my tuition even when the scholarship was ending they said Sarah, we are paying for two years at ago and paid for the field’s activities,” she recalls.
She is equally grateful to everyone who provided her and her research team with useful information; Kyambogo University for assigning a teaching assistant to help her focus and her husband, Dr. Bunoti, who has promised to support her dream.
“I want to thank my family, my sister Mrs. Rebecca Lucy and her husband Eng. Dr James Muwuluke, my children. They have been there for me, my husband, Dr. Bunoti met me when I was a primary school teacher and he was a Doctor teach and told me, Sarah, I will support you until you are tired of reading and has kept his word, there are few empowered men who will want a woman to come up and get the title they hold,” she said.

“Given what I have gone through, am so excited about this achievement. My family is so excited about this. My husband is extremely excited. They have written short paragraphs about me about my resilience. I had decided not to hold any celebration but my sister and her husband says this could not pass since it is no mean achievement,” she says.
Dr. Godfrey Siu Etyang, her Ph.D. overseer, has invited her to collaborate on a parenting project at the Child Health and Development Center, College of Health Sciences, Makerere University. Over the past month, she has been actively contributing to the development of a comprehensive parenting curriculum for the unit.
Dr. Bunoti anticipates scaling up the approved intervention, particularly to additional primary schools in the Busoga region and beyond and has already began talks with Ministry of Education and Sports to support children’s understanding of puberty, a sine qua non for education and parenting.
Unexpected difficulties affected Dr. Sarah Bunoti Nantono’s journey to earning her Ph.D., resulting in longer than the expected four to six years. Midway through her studies, she developed insomnia, which was an unexpected health problem. In 2020 when it appeared that she would soon graduate, the Doctoral Committee insisted that she must publish her work, and was reluctant to accept a monograph, one of the options for one to graduate with a PhD at Makerere University. Further delays were due to lengthy processes to have her manuscripts published and clearances through the Institutional Review Board (IRB). Other than these challenges, Dr. Nantono also had to repeat the entire data collection process and deal with the untimely death of Assoc. Prof. Joseph Oonyu, a key member of her doctorate committee, in October 2020. Despite these challenges, Dr. Nantono feels proud to have completed her doctorate, demonstrating her incredible endurance in the face of adversity.
Congratulations Sarah!
You may like
-


Mak News Magazine: February 2026
-


Celebrating Academic Excellence: CoBAMS Presents 975 Graduands at Mak 76th Graduation Ceremony
-


Mak 76th Graduation Ceremony: CoNAS Presents 16 PhDs & Best Performing Male Student in the Sciences
-


Medical graduates urged to uphold Ethical values
-


CAES Presents Overall Best Performing Student in the Sciences & a Record 28 PhDs at the 76th Graduation Ceremony
-


Over 9,200 to graduate at Makerere University’s 76th Graduation
Health
MakSPH Environmental Health Graduates Trained to Prevent Disease at Its Source
Published
6 days agoon
February 24, 2026
In most health systems, attention turns to illness after it appears in clinics and hospitals. Environmental Health works earlier, often invisibly, by preventing disease before treatment becomes necessary. At Makerere University School of Public Health (MakSPH), this preventive philosophy shapes the training of students learning to manage health risks at their source, through sanitation systems, safer environments, community engagement, and evidence-based public health action.
This year, as MakSPH presents 29 graduands approved by the Makerere University Senate for the award of the Bachelor of Environmental Health Science (BEHS) degree, four outstanding students graduate with first-class honours. Their journeys, shaped by different personal histories and professional ambitions, provide a clear view of how the School prepares practitioners whose work begins long before patients reach health facilities. Through academic training, field practice, research exposure, and leadership experience, the programme equips graduates to address the environmental and social conditions that determine health outcomes across communities.

Environmental health occupies a distinctive position within public health practice. Rather than focusing primarily on diagnosis or treatment, practitioners work at the intersection of science, policy, and society, addressing risks linked to water and sanitation, food safety, occupational health, climate change, and urbanisation. The discipline demands technical competence alongside communication, systems thinking, and community engagement, capabilities that increasingly define modern public health leadership.
The journeys of Nakulima Bushirah, graduating with a CGPA of 4.58 on February 25, 2026, Mujurani Alphersiiru with 4.44, and Cherop Eric with 4.41, alongside Phillip Acaye, the cohort’s overall best student with a CGPA of 4.63, demonstrate how MakSPH shapes students from varied beginnings into professionals grounded in prevention. Their paths reveal a shared formation that links classroom learning with real-world health challenges and prepares graduates to prevent disease before it occurs.
Bushirah Nakulima’s Turn Toward Prevention

For Bushirah Nakulima, environmental health began during a period of uncertainty. The COVID-19 pandemic repeatedly disrupted her Bachelor of Pharmacy studies at Kampala International University, prompting reflection about the kind of health professional she wanted to become. A conversation with a family friend working in preventive health introduced an alternative path, one focused not on treating illness after onset but on preventing it altogether.
“When I applied to Makerere University in 2022, I was considering two career paths,” she recalled. “I prayed to Allah to guide me toward the best one. When I was admitted to the Bachelor of Environmental Health Science, I accepted it wholeheartedly, and I came to appreciate it even more as I studied.”
Her academic foundation had already demonstrated consistency. She progressed from Melody Junior School in Nansana, where she obtained aggregate eight in 2010, to Shuhada’e Islamic School in Nyamitanga, completing O-Level with 25 aggregates in 2016 and A-Level with 10 points in 2018. Pharmacy initially appeared the logical continuation, yet environmental health offered something broader in scale and impact.
“Environmental Health offered an opportunity to prevent illness and suffering before it occurs,” she explained. “It allows a single intervention, such as WASH or health education, to protect many people at once, and it provides flexibility to work across diverse environments. It offered freedom to operate in various settings, which truly connects with my personality since I love exploration.”
At MakSPH, classroom concepts quickly translated into practice. During her internship at Mukono Municipal Council, she conducted school health education sessions, participated in inspections of markets and abattoirs, and engaged communities facing sanitation challenges. Field exposure deepened her understanding of how environmental conditions directly shape disease patterns, reinforcing prevention as both a scientific and social responsibility.
Leadership further expanded her training. Serving as the 90th Female Guild Representative Councillor (GRC), she represented the School of Public Health in the Student Guild structure, facilitating engagement between students and School leadership on academic and welfare matters. The role strengthened her capacity for representation, negotiation, and collaborative problem-solving, skills central to public health practice, where advocacy and systems engagement are inseparable from technical expertise.
Graduating with a CGPA of 4.58, Bushirah’s research examined roadside vendors’ exposure to air pollution in Kampala, reflecting growing concern about occupational and urban environmental risks. She now plans to pursue advanced training in public health, building on MakSPH’s emphasis on evidence-driven and community-centred practice.
Cherop Eric’s Return to the Classroom

Eric Cherop’s journey into environmental health began not in lecture halls but in community service. Raised in Kapchorwa District, he was shaped by economic hardship and resilience, experiences that informed his commitment to community well-being.
He completed his Primary Leaving Examinations at Chema Primary School, a Universal Primary Education institution, attaining 24 aggregates in 2008. He later joined Sipi Secondary School, where he obtained 37 aggregates at Uganda Certificate of Education in 2012 and continued at the same school for A-Level, earning 8 points at Uganda Advanced Certificate of Education in 2014.
After earning a Diploma in environmental health sciences from Mbale School of Hygiene between 2015 and 2017, he entered public service as an Environmental Health Officer and Community Field Facilitator with Kapchorwa District Local Government. His work included sanitation campaigns, climate resilience initiatives, nutrition education, and household behaviour change programmes. Over time, field experience revealed the limits of practice without deeper theoretical grounding.
“I wanted to understand not only what works in communities, but why it works,” he explains. Enrolling in the BEHS programme at MakSPH in 2022 allowed him to connect practical experience with analytical training. Coursework strengthened competencies in environmental risk assessment, participatory engagement, and data-driven planning. Mentorship reshaped how he interpreted evidence.
“My lecturers helped me move beyond seeing data as numbers,” he said. “I learned to see it as evidence that guides decisions and improves accountability.” Graduating with a CGPA of 4.41, Eric now aims to advance evidence-driven leadership at the intersection of climate change, nutrition, and environmental health, ensuring interventions remain grounded in community realities.
Mujurani Alphersiiru’s Path into Environmental Health

For Mujurani Alphersiiru, Environmental Health arrived at an unexpected moment, when his academic future appeared uncertain. Financial pressures had begun to threaten the continuation of his Bachelor of Nursing Science studies at Kampala International University Western Campus, raising the real possibility that his university education might end prematurely. The turning point came when the government district quota admission list was released, offering him placement at Makerere University under Bunyangabu District and opening an alternative academic pathway he had not previously considered.
At the time, environmental health was unfamiliar to him. “I didn’t know what environmental health was,” he recalls. “But I celebrated because I had reached my dream university.” Orientation sessions and early coursework gradually reframed that uncertainty, revealing a discipline grounded in prevention, systems thinking, and public health policy. What began as an unexpected opportunity soon developed into a clear professional direction.
Serving as class president and 90th Male GRC for the School with Nakulima Bushirah, Mujurani organised student activities, mobilised community outreach initiatives, and advocated for improved learning environments. Balancing leadership responsibilities with academic performance required deliberate discipline and time management.
His educational foundation began at St. Augustine Butiiti Demonstration Primary School in Kyenjojo, where he scored 12 aggregates in 2014. He later attended Pride Secondary School in Mityana, attaining 25 aggregates at O-Level in 2018, before proceeding to Kibiito Secondary School in Bunyangabu, where he obtained 13 points at A-Level in 2021, performance that earned him government sponsorship for university education. At MakSPH, faculty mentorship further strengthened both his academic rigour and commitment to public service.
“Government sponsorship meant responsibility,” Mujurani said. “I had to plan my time carefully while remaining active in school programmes.” Graduating with a CGPA of 4.44, his interests now centre on governance and accountability within health systems, particularly strengthening the implementation of public health policies.
Training Prevention Professionals
Taken together, the three journeys demonstrate how MakSPH’s Environmental Health training converts diverse personal backgrounds into a shared professional orientation centred on prevention. Through interdisciplinary coursework, field placements, research mentorship, and leadership opportunities, students develop competencies that extend beyond technical knowledge to include systems thinking and public engagement.

The BEHS programme, established in 2000 within MakSPH’s Department of Disease Control and Environmental Health, remains the School’s only undergraduate degree and has trained more than 1,000 graduates who now serve across government institutions, non-governmental organisations, academia, and international health programmes. Its continued evolution reflects growing recognition that strengthening health systems requires professionals capable of addressing environmental risks before illness occurs.
The achievements of this year’s graduates, therefore, represent more than academic distinction. They reflect a model of training designed to prepare professionals whose work reduces the need for treatment by preventing disease at its source, reinforcing MakSPH’s role in shaping Uganda’s environmental health workforce.
Health
Philliph Acaye and the Making of Uganda’s Environmental Health Workforce
Published
6 days agoon
February 24, 2026
As Makerere University School of Public Health (MakSPH) presents 29 graduands on February 25, 2026, at Makerere University’s 76th Graduation Ceremony, for the conferment of the Bachelor of Environmental Health Science (BEHS) degree, the journey of the cohort’s best student provides a compelling window into both individual resilience and institutional impact. Philliph Acaye, graduating with a CGPA of 4.63, represents more than academic distinction. His story reflects the lived realities that shape many public health professionals in Uganda and shows how rigorous training can transform experience into leadership within health systems.

Education Shaped by Conflict
Acaye was born on October 2, 1993, in Wangduku Village, Palenga Parish, Pajule Sub-County, Pader District in northern Uganda, a region deeply affected by the Lord’s Resistance Army (LRA) insurgency in the early 2000s, where education and security often existed in constant tension. As a child, schooling unfolded alongside displacement and uncertainty, conditions that shaped an entire generation growing up during the conflict.
“Around 2002, before we had fully moved into the IDP camps, we often ran with our parents whenever there were LRA attacks,” he recalls. “But on several occasions, they caught us unaware. During one of the attacks, they abducted me and moved with me for close to seven kilometres, from Wangduku to Pajule Trading Centre in Pader. At first, they said I was too young to be moved with. I was around nine or ten years old. Later, I understood that someone among them personally knew my father and did not want me taken, so he used my age as the reason, and they left me behind.”

He narrates that several relatives and neighbours, including some of his childhood friends, were not spared, among them an uncle whose whereabouts remain unknown to this day. “If they had gone with me,” Acaye reflects quietly, “I could be dead, or I might not have studied.” The remark sits deep and places his graduation in context, not simply as personal success, but as the outcome of persistence through years when conflict repeatedly disrupted education across northern Uganda.
Between 2002 and 2006, his schooling continued inside Pajule Internally Displaced Persons (IDP) Camp, where families lived in overcrowded settlements and depended largely on relief food. Learning environments were unstable, teachers travelled under risk, and lessons were frequently interrupted by insecurity. Even within the camps, attacks remained possible. Education progressed slowly, but it continued, sustained by families and teachers who insisted that schooling remained essential despite uncertainty.
When communities gradually returned home, Acaye rebuilt his academic track record step by step. He completed Primary Leaving Examinations in 2007 with an aggregate of 19 and was the best pupil at Wangduku Primary School, at a time when enrolment remained low because many families feared returning to villages. He proceeded to Pajule Senior Secondary School, completing O-Level in 2011 with 31 aggregates, and later obtained 10 points at A-Level in 2013 from Kitgum High School.
However, his progression was shaped by consistent recovery after disruption, supported by relatives, teachers, community mentors, and educational assistance from Invisible Children, a post-LRA conflict recovery NGO led locally by Ms. Laker Jolly Okot, which supported his A-Level education.
Professional direction emerged during his training at the Mbale School of Hygiene, where he pursued a Diploma in Environmental Health Science from 2014 to 2016 and graduated with a strong CGPA of 4.4. The diploma opened immediate employment opportunities in community and humanitarian health settings back home, followed by service in local government. Today, he works as a Health Inspector in Kitgum District Local Government, implementing sanitation monitoring, infection prevention activities, and community health interventions. Practical experience strengthened his understanding of public health challenges but also revealed limits in technical depth that he felt required further training.
Training the Public Health Professional
His admission to MakSPH in 2022 through the government diploma-entry sponsorship scheme represented a deliberate academic decision rather than a career reset. He sought broader analytical skills and a stronger grounding in environmental health systems, particularly in areas of surveillance, planning, and evidence-based decision-making.
“I realised some technical aspects were not fully covered at the diploma level. I wanted to understand public health beyond implementation and learn how decisions are justified scientifically,” Acaye explained.

The sponsorship, he observed, transformed that ambition into possibility and remains central to how he understands his academic journey at Makerere University. “I am grateful to the Makerere University selection committee, the MakSPH selection committee, and the Government of Uganda for this opportunity. Opportunities like this are not guaranteed, and I recognise the trust placed in me to undertake and complete the three-year BEHS programme.”
The transition into university study was not seamless, though. His admission had come earlier than planned, and he began coursework without formal study leave while still tied to workplace obligations in Kitgum. Sustained support from district leadership, particularly Dr. Okello Henry Otto, the District Health Officer, eventually enabled him to secure study leave and concentrate fully on academic work. Now with stability came rapid academic improvement, supported by peer learning, faculty mentorship, and a strong curriculum that emphasised analytical reasoning alongside applied practice.
Acaye attributes his transformation to the programme’s academic culture rather than individual brilliance. “The programme helped me realise that what I was doing before was only a surface understanding,” he argued. “I learned to approach public health more deeply.” Exposure to research methods, he revealed, reshaped how he interpreted field experience and encouraged him to submit an abstract to an international academic conference, marking his transition from practitioner to emerging researcher.
For Mr. Abdallah Ali Halage, the MakSPH Coordinator of the BEHS programme, such outcomes reflect intentional design rather than coincidence. He noted that student success is rooted in a training philosophy that combines technical instruction with professional discipline from the moment students enter the programme. According to him, orientation focuses not only on coursework but also on expectations of conduct, independence, and responsibility. “When students join, we brief them on how seriously they must approach their academic journey,” he said. “That grounding helps shape their performance over time.”

Mr. Halage argued that while some high-performing students enter through diploma schemes, achievement ultimately depends on commitment and effort rather than background. He cited Acaye’s consistent curiosity and self-motivation as defining traits, noting that strong academic results tend to follow students who actively engage with the learning process.
“I congratulate Philliph and his colleagues upon attaining first-class honours and performing very well academically. Philliph has been hardworking and self-motivated. He has consistently shown a strong interest in his studies, and that commitment has helped him achieve this result. He has been a very good student,” Mr. Halage attested.
He added that the achievement reflects a broader culture within the programme. “Our students are disciplined and independent. Their commitment, together with support from the School management, the College and University leadership, has contributed greatly to their success.”

From Individual Achievement to Institutional Impact
The broader significance of Acaye’s achievement becomes clearer when placed within the evolution of the BEHS programme itself. Established in 2000 within MakSPH’s Department of Disease Control and Environmental Health (DCEH), the programme remains the School’s sole undergraduate degree and was among the earliest environmental health bachelor’s programmes in East Africa. In more than two decades, it has produced over 1,000 graduates, expanding professional capacity beyond diploma-level training and strengthening Uganda and the region’s environmental health workforce across government, non-governmental organisations, educational institutions, and points of entry such as airports and border services.
Mr. Halage explained that the programme helped redefine career pathways within the government of Uganda’s public service structures by introducing degree-level expertise into environmental health roles. Graduates now serve as Environmental Health Officers, Senior Environmental Health Officers, and technical specialists contributing to policy implementation and service delivery across multiple sectors. The academic pathway has also expanded vertically, with postgraduate training opportunities at MakSPH currently enabling graduates to progress into research, teaching, and doctoral-level specialisation, ensuring continuity within the discipline.

A Programme Shaping Regional Practice
The reputation of Makerere University’s Bachelor of Environmental Health Science programme is also increasingly influencing regional institutions. During a strategic benchmarking visit to MakSPH on July 30, 2025, Dr. Ratib Dricile, Dean of the Faculty of Health Sciences at Muni University, described the School of Public Health as a reference point for universities seeking to strengthen environmental health training in the region.
The main reason the delegation visited Makerere University School of Public Health was that Muni University remains a young and growing institution located in north-western Uganda along the borders with the Democratic Republic of Congo and South Sudan, where porous borders contribute to frequent cross-border diseases, many of which are preventable through strong environmental health approaches, Dr. Dricile explained.

“Makerere University, with over 100 years of institutional experience and 25 years running the Environmental Health programme, was the right place for us to benchmark, particularly in curriculum design, course content, programme structure, and implementation,” he said. “We were impressed by the work being implemented and gained more than we initially expected. By integrating these experiences, we believe the Muni University curriculum can become even stronger. The collaboration will allow us to adopt innovations built on Makerere’s long experience, and we believe that working together with Makerere University will strengthen Muni University institutionally and contribute positively to our university’s growth and ranking.”
It is within this institutional tradition, built over decades of training environmental health professionals across Uganda and the region, that Philliph Acaye’s achievement takes meaning. For him, graduating top of the class remains grounded in practical purpose rather than prestige. He views a first-class degree as an opportunity rather than an endpoint. Recalling guidance from his lecturers, he said strong academic results can open doors but must be followed by demonstrated competence. “A first class helps you get shortlisted,” he said. “After that, you must prove yourself.”

His immediate plans reflect that perspective. He is currently pursuing additional training in Health Services Management at Gulu College of Health Sciences while preparing for postgraduate study in either public health or environmental and occupational health. At the same time, he continues supporting pupils in his community and plans to mobilise resources to provide sanitary pads for girls at his former primary school, an initiative he believes will help reduce school dropout rates in rural areas.
Acaye’s journey, from disrupted schooling in an IDP camp to graduating top of MakSPH’s BEHS programme for the 2022 cohort, reflects the deeper purpose of public health education. As MakSPH presents its newest cohort for graduation this week, his story demonstrates how the programme turns lived experience into professional capacity, strengthening communities and health systems across Uganda and the region, one graduate at a time.
Health
Makerere University School of Public Health Graduates First Cohort of Cost-Effectiveness Analysis Short Course
Published
1 week agoon
February 20, 2026By
Mak Editor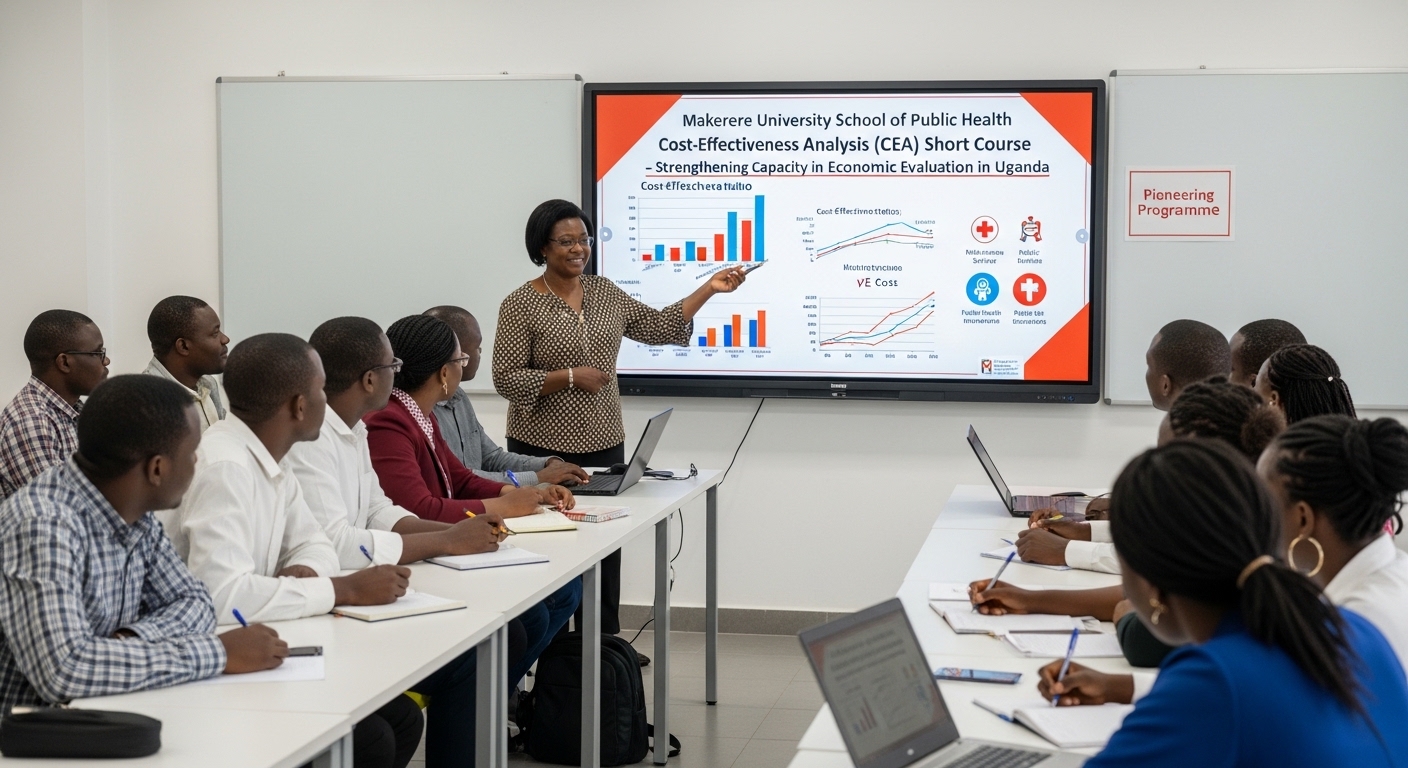
Kampala, Uganda – The Makerere University School of Public Health (MakSPH) has marked a significant milestone with the graduation of the first-ever cohort of its Cost-Effectiveness Analysis (CEA) Short Course. The pioneering programme is designed to strengthen capacity in economic evaluation in Uganda and beyond.
The virtual graduation ceremony honored eleven (11) participants who completed the course. The cohort included professionals from academia, research institutions, government agencies, and non-state actors, reflecting the increasing demand for skills in economic evaluation across sectors.
The short course was developed and implemented by the Department of Health Policy, Planning, and Management (HPPM) in response to the increasing need for evidence-informed decision-making in a context of limited resources.
In her remarks during the ceremony, Assoc. Prof. Suzanne Kiwanuka, Head of the Department of Health Policy, Planning and Management (HPPM) at MakSPH, congratulated the inaugural cohort for completing what she described as a “critical and timely” course.
“With decreasing resources and rising demand for services driven by population growth and the emergence of high-cost technologies, decision-makers must make difficult choices,” she noted. “Cost-effectiveness analysis is no longer optional. It is central to conversations in the corridors of power.”
The CEA short course was designed to equip policymakers, researchers, and practitioners with both theoretical knowledge and practical skills in economic evaluation. Participants were introduced to key principles of health economics, costing methodologies, decision-analytic modelling, Markov modelling, sensitivity analysis, and interpretation of incremental cost-effectiveness ratios (ICERs).
According to Prof. Elizabeth Ekirapa, the course lead at MakSPH, this inaugural offering had been “a long time coming,” following years of discussions within the department about building local expertise in economic evaluation.
Delivered over 10 days through interactive online sessions, the course combined lectures, case studies, and hands-on modelling exercises using contextually relevant datasets. Participants were required to develop and present applied cost-effectiveness projects as part of their assessment, allowing them to translate theory into practice.
During the feedback session at the graduation ceremony, faculty emphasized the importance of clarity in defining study perspectives, selecting appropriate outcomes, and aligning research questions with modelling approaches.
Dr. Chrispus Mayora, one of the facilitators, highlighted the need to carefully select outcomes that directly reflect the intervention being evaluated. “When thinking about outcomes, ask yourself: Is this aligned with what I want to study? Interesting outcomes are not always the most appropriate ones,” he advised.
Participants were also encouraged to select modelling techniques such as decision trees or Markov models based on the research question and the nature of the disease or intervention under study.
Prof. Ekirapa described the graduates as “trailblazers,” noting that their feedback would shape future iterations of the course. “When you are the first cohort, you are like pioneers,” she remarked. “We are committed to improving this course to ensure it becomes a world-class programme.”
For many attendees, the graduation ceremony was a new experience, as certificates were awarded virtually an approach that participants welcomed as innovative and inclusive.
“Cost-effectiveness analysis enables us to maximise value for money,” noted Dr. Crispus Mayora of MakSPH. “It allows decision-makers to compare interventions systematically and ensure that limited resources achieve the greatest possible benefit.”
The programme aligns with Makerere University’s broader mandate to provide high-quality training that responds to national and regional development priorities. Participants who successfully complete the course receive a certificate signed by the Dean of the School of Public Health.
As the ceremony concluded, faculty encouraged continued engagement beyond the classroom. Graduates were urged to refine their project ideas and collaborate with the department in advancing research and policy discussions.
The successful completion of the first CEA short course marks an important step in building a cadre of professionals equipped to conduct rigorous economic evaluations. With plans to expand and refine the programme based on participant feedback, the HPPM department under MakSPH is positioning itself as a regional leader in health economics and policy analysis training.
Trending
-

 Humanities & Social Sciences7 days ago
Humanities & Social Sciences7 days agoMeet Najjuka Whitney, The Girl Who Missed Law and Found Her Voice
-

 General6 days ago
General6 days ago76th Graduation Highlights
-

 Health2 weeks ago
Health2 weeks agoUganda has until 2030 to end Open Defecation as Ntaro’s PhD Examines Kabale’s Progress
-

 Agriculture & Environment1 week ago
Agriculture & Environment1 week agoUganda Martyrs Namugongo Students Turn Organic Waste into Soap in an Innovative School Project on Sustainable Waste Management
-

 General2 weeks ago
General2 weeks agoMastercard Foundation Scholars embrace and honour their rich cultural diversity
