Health
MakCHS Student Innovation shines at HIHA 2021
Published
4 years agoon
By
Zaam Ssali
A team of students led by Ms. Anna Maria Gwokyalya – 4th year student of Medicine and Surgery at the College of Health Sciences (MakCHS), Makerere University won the award of ‘Student Innovation of the Year’ at the Heroes in Health Awards (HIHA) held on the 12th November, 2021. Her innovation was a book “The Mugishas’ COVID-19 Tale” designed to help children be more involved in the fight against the Covid-19 pandemic.
Inaugurated in 2019, The Heroes in Health Awards (HIHA) is a public private initiative adopted by the Ministry of Health with the support of Xtraordinary Media to offer opportunity to members of the public to motivate Uganda’s excellent health sector players, recognize and encourage new innovations that will transform our health care system.
Anna Maria shares the experience of the team in an interview below:
Tell us more about your team
We are a team of five students who have worked on numerous research projects and online campaigns to increase awareness of Antimicrobial Resistance under ARSU (Antimicrobial Resistance Stewardship Uganda). Whereas I was the leader of this comic book project, it’s the brainchild of the entire team, an indicator of respect, mutuality and friendship.
Describe your innovation and what motivated you to work on it
This book entitled, “The Mugishas’ COVID-19 Tale” contains fascinating illustrations with simplified information on symptoms, transmission and prevention of COVID-19 that includes both observation of the standard operating procedures and vaccination.
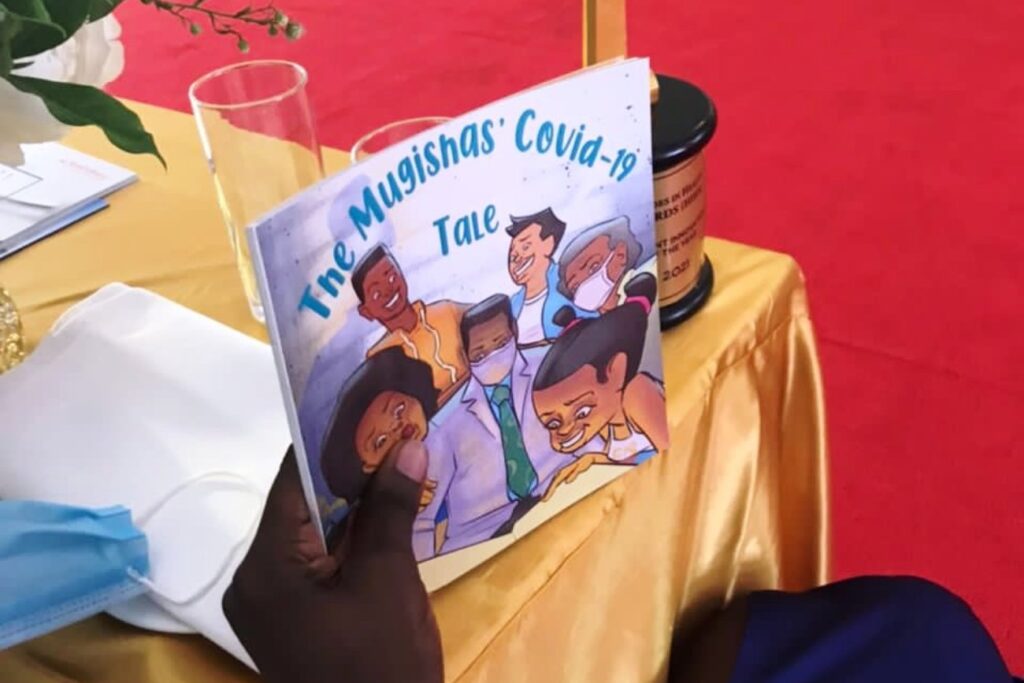
The book is a means of creating awareness on COVID-19 disease and its prevention among children below 12 years, a vulnerable group that is not eligible for vaccination (as per Uganda’s Vaccination Guidelines) against this disease, we designed the book to help children be more involved in the fight against this disease.
Infection prevention and control is not only pertinent to fighting Antimicrobial Resistance but also to promotion of health and wellbeing of the people. Writing this book is our contribution to controlling of infection as well as prevention, an important aspect of primary health care.
What is the impact of the book from your perspective?
Since the comic book is very illustrative and appealing to the eye, we anticipate that the children will gain knowledge on COVID-19 as they enjoy the illustrations. We also hope that they will be agents of change through sharing this knowledge with their peers both at home and at school, protecting them against the disease in the long run.

What is your advice to others about new ideas and innovations?
My advice is drawn from two quotes;
Quote 1: “Find something you’re passionate about and keep tremendously interested in it.” – Anonymous
Quote 2: “Teamwork is the secret that makes common people achieve uncommon results” –Ifeanyi Enoch Onucha
Innovations by MakCHS Research teams were exhibited at the HIHA Awards as well. These included:
VITEX (Medical Assistance Tool): Vitex is an integrated system that utilizes antimicrobial and affordable 3D plastics made out of 80% waste plastic, making it eco-friendly. The device sterilises wards up to 99.9%, thus preventing nosocomial infections by employing powerful pulsating U.V engine and spots latest in artificial intelligence to improve patient care and practitioner assistance.

Vitex is intended to improve health professionals’ quality of work by reducing workload and deters transmission of highly contagious infections such as COVID-19. It also improves access to vital medical literature, facilitates electronic consultation, service delivery in the medical environment, including carrying out consistent patient monitoring and reducing prescription/medication errors.
The device spots a Powerful Artificial Intelligence package that incorporates Intel RealSense, auto-follow, video capture, touch & voice control, playful expressions, and personality to keep patients in a cheerful mood. Vitex includes over-the-air updates making it viable for endless integration, including providing seamless data access for important time-sensitive decision-making through elaborate integrations.

Team: Dr. Justine Nnakate Bukenya (PI), Ainembabazi Samantha, Joeltta Nabungye, Kiirya Arnold, Mugisha Gift Arnold
The Early Preeclampsia Detection Strip (EPED Strip): The Early Preeclampsia Detection (EPED) Strip is a urine-based point-of-care detection strip for preeclampsia that pregnant women can use at home to self-screen for the condition. Preeclampsia is a maternal condition characterized by high blood pressure of 140/90mmHg and proteinuria after 20 weeks of pregnancy. Worldwide the condition is responsible for over 500,000 infant deaths and 70,000 maternal deaths annually. By seeking medical care at the early onset of preeclampsia, the condition can be appropriately monitored and controlled, thereby reducing the detrimental health impacts of undiagnosed preeclampsia which is a health burden to LMICs. Thus, the EPED strip is being designed to diagnose this condition early and functions very similar to a pregnancy test where urine is applied to one end of the strip, and pulled across it by capillary attraction to where antibodies specific to the biomarkers are immobilized. In the reaction matrix there are two lines, a test line and a control line. The presence or absence of the control and test lines indicates the presence or absence of the captured conjugates. This is designed with adaptation from the existing lateral flow assay (LFA) technology. While the primary goal of the EPED strip is to be a home-based early detection tool, the EPED strip can also be used to assist the diagnosis of preeclampsia in a clinical setting from large-scale national hospitals to remote health clinics.
Team:Prof Paul Kiondo (PI), Brian Matovu, Zoe Ssekyonda, Calvin Abonga, Olivia Peace Nabuuma, Dr. Robert Ssekitoleko
The Maternal PPH Wrap: The maternal PPH wrap; a wearable device strapped around the mother’s waist; affordable compared to the other devices that is able to carry out external compression of the uterus through the abdominal wall in order to stimulate myometrium contraction. The design is based on already used bimanual uterine compression techniques which are manually done by qualified and skilled personnel.
Despite the number of interventions, postpartum haemorrhage still remains the leading cause of maternal death globally. Most of the interventions that are recommended under standard clinical practical guidelines such as uterotonic drugs, therapeutic devices or even surgery are unavailable in the communities of low and middle income countries including Uganda simply because they are unaffordable and most times require qualified/skilled personnel and highly sterile environments.
The device will rely on an inflatable rubber bag to provide the pressure to do the sustained compression. The inflation will be done using a bulb similar to the one used by a sphygmomanometer. This is way less labour intensive than the procedure of bimanual uterine compression. The overall aim Is to create an efficient device that is affordable in Uganda and all developing countries’ healthcare markets as a leading lifesaver of mothers.
Team: Owen Muhimbisa, Kiwanuka Martin, Arinda Beryl, Maureen Etuket, Denis Mukiibi, Robert Ssekitoleko.
Zaam Ssali is the Principal Communication Officer SoL & MakCHS
You may like
-


Makerere Graduation Underscores Investment in Africa’s Public Health Capacity
-


Makerere’s 76th Graduation Ceremony: CHS showcases research strength with 26 PhD Graduates
-


Medical graduates urged to uphold Ethical values
-


Philliph Acaye and the Making of Uganda’s Environmental Health Workforce
-


76th Graduation Highlights
-


Olivia Nakisita and the Quiet Urgency of Adolescent Refugee Health
Health
Makerere Graduation Underscores Investment in Africa’s Public Health Capacity
Published
3 days agoon
March 4, 2026
KAMPALA, 25 February 2026 — Higher education must move beyond awarding degrees to producing solutions for national and global crises, speakers said on Wednesday as Makerere University continued its 76th Graduation Ceremony, positioning universities as central actors in strengthening Africa’s public health capacity.
Addressing graduands on Wednesday, February 25, 2026, at Freedom Square, national leaders and university officials framed graduation not as a ceremonial endpoint but as an investment in workforce readiness, research leadership, and evidence-driven governance, particularly at a time when health systems across the continent face growing pressure from pandemics, demographic change, and climate-related risks.
The message resonated strongly through presentations from Makerere University School of Public Health (MakSPH) and Makerere University College of Health Sciences (MakCHS), whose graduates enter professional service amid renewed global attention to health system resilience, scientific leadership, and locally generated research.
Delivering the commencement address on Day Two of Makerere University’s 76th Graduation Ceremony, Dr. Margaret Blick Kigozi, Board Chairperson of the Makerere University Endowment Fund, reflected on her graduation in 1976 during a period of national uncertainty under then-Chancellor President Idi Amin. She recalled leaving Uganda soon after with her young family, carrying “little more than education, values, and hope,” an experience she used to frame lessons on resilience, purpose, and responsibility in uncertain times.

Challenging graduates to rethink professional success, she reminded those entering health and life sciences that their training carries extraordinary influence.
“Power does not make you important; it makes you responsible,” she said. “You will decide who is listened to and who is dismissed, who waits and who is rushed through, who feels safe and who feels small. Your education has trained you to ask better questions, but your humanity must guide the answers. Behind every chart, every case, every experiment, there is life, and life deserves care, patience, and dignity.”
Throughout the ceremony, speakers returned to a common refrain: societies increasingly depend on evidence, and universities must produce professionals capable of translating knowledge into policy, practice, and community impact.
Across the four-day congregation, the University will award 9,295 degrees and diplomas, including 2,503 Master’s degrees, 6,343 Bachelor’s degrees, 206 Postgraduate Diplomas, and 30 Diplomas. But beyond the numbers, speakers repeatedly returned to a central question on how higher education can translate academic growth into national development and health security.
On day two, graduands were presented from the College of Natural Sciences, the College of Veterinary Medicine, Animal Resources and Biosecurity, the College of Health Sciences, and the MakSPH, the latter positioned squarely within Africa’s ongoing struggle to expand its pool of trained epidemiologists, health systems researchers, and policy leaders.
Vice Chancellor Prof. Barnabas Nawangwe noted that Africa averages just 80 researchers per million people, compared to a global average of 1,081, warning that the human resource gap remains substantial.
“Today the School of Public Health presents graduands joining the field at a time when Africa faces a critical shortage of highly trained public health leaders,” he said.

The School of Public Health presented seven PhD candidates: Aber Harriet Odonga, Komakech Henry, Lubogo David, Nakisita Olivia, Namukose Samalie, Ntaro Moses, and Osuret Jimmy. It also graduated 195 Master’s students and 29 Bachelor of Environmental Health Science graduates, including four first-class honours recipients led by Phillip Acaye with a CGPA of 4.63.
Their research spans maternal and child health, epidemic preparedness, sanitation behaviour change, nutrition systems integration, and injury prevention, areas increasingly recognised as foundational to national development rather than peripheral health concerns.
University Chancellor Dr. Crispus Kiyonga emphasized that research must move beyond academic publication into policy and implementation.
“Research plays a very vital role in the development of any community,” he said, linking university scholarship directly to Uganda’s national development agenda.

For public health education, that responsibility carries particular urgency. The COVID-19 pandemic, recurring disease outbreaks, and climate-linked health risks have exposed how deeply national stability depends on scientific capacity.
The chancellor hailed the Government of Uganda for committing UGX 30 billion through the Makerere University Research and Innovations Fund (MakRIF).
Mak Urged on More PhDs
Representing the First Lady and Minister of Education and Sports, State Minister Dr. Joyce Kaducu Moriku described doctoral training as central to Uganda’s research ambitions, noting government efforts to expand funding and modernize higher education systems.

“Universities must produce more PhDs to strengthen the national research agenda,” she said, adding that competence-based reforms aim to align training more closely with societal needs.
“More PhDs also mean the university is growing in academic leadership and an increase in research. So, keep the numbers growing, especially in Science, Technology, and Engineering,” she added.
The 213 PhDs conferred this year, a record, signal more than institutional expansion but a response to structural deficits.
Africa bears approximately 25% of the global disease burden but produces a disproportionately small share of global health research. The continent’s research density remains far below global averages. In this context, each doctoral graduate becomes not merely an academic achievement but a strategic asset.
A University Responding to Its Moment
For the School of Public Health, the graduation reflects a broader evolution in how public health training is conceived. Rather than focusing solely on the treatment of disease, the field increasingly addresses systems, sanitation, nutrition, behavioural change, surveillance, prevention, and climate change, areas where research directly shapes everyday life.
Recent MakSPH-led initiatives, including national HIV impact surveys and digital health system expansion, demonstrate how academic institutions increasingly function as implementation partners to the government rather than observers.
Over the past five years, MakSPH has supported the national scale-up of electronic medical records through the CDC-funded Monitoring and Evaluation Technical Support (MakSPH-METs) programme, and led the Third Uganda Population-Based HIV Impact Assessment (UPHIA 2024–2025), the first fully Ugandan-implemented national survey of its kind.
Launched in 2020, the METs program has supported the nationwide scale-up of UgandaEMR+, transitioning thousands of facilities to secure electronic medical records and deploying critical ICT infrastructure. In March 2026, these systems will be formally transitioned to the Ministry of Health, reflecting sustainable national ownership.
Health
Three MakSPH Faculty Honoured with Makerere University Research Excellence Awards 2026
Published
4 days agoon
March 2, 2026
KAMPALA—Three faculty members from Makerere University School of Public Health (MakSPH) have been recognised at the Makerere University Vice-Chancellor’s Research Excellence Awards 2026, highlighting the School’s expanding contribution to research leadership, scientific productivity, and policy-relevant scholarship across Africa.
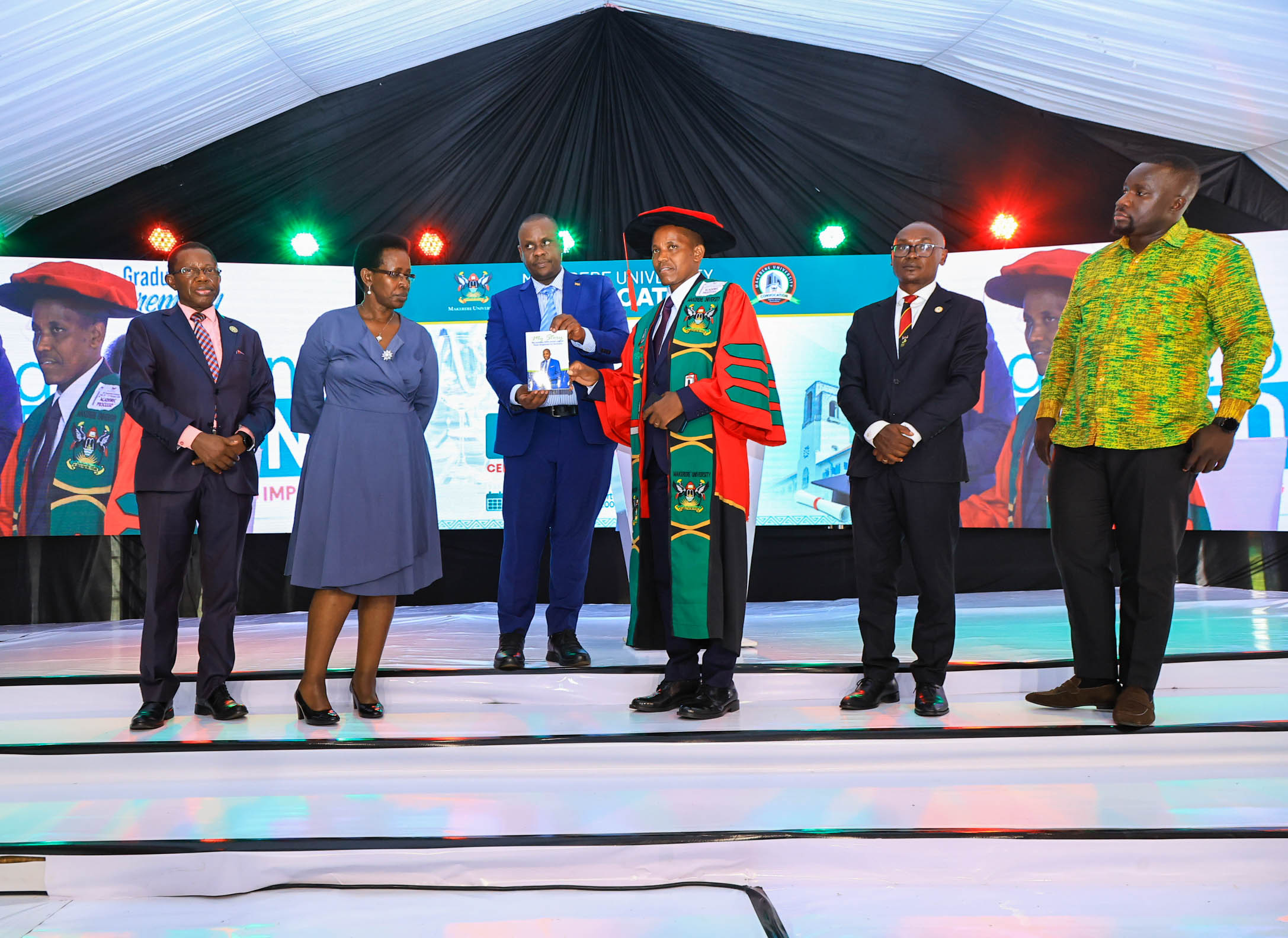
Associate Professor Peter Kyobe Waiswa, Associate Professor David Musoke, and Juliana Namutundu received honours during the University’s 76th Graduation Ceremony at Freedom Square, where Makerere celebrated scholars whose work has demonstrated exceptional research achievement and impact beyond academia.

The annual awards, coordinated by the Directorate of Research, Innovation and Partnerships (DRIP), recognise faculty and staff whose scholarly output and leadership advance Makerere University’s ambition to become a research-led institution.
“This recognition celebrates sustained excellence in research productivity and contributions to knowledge that advance both national and global discourse,” Vice-Chancellor Prof. Barnabas Nawangwe said. “We are strengthening a culture where research does not remain confined to journals but translates into solutions for society.”
Among the university’s top researchers was Assoc. Prof. Peter Kyobe Waiswa, a health systems scientist whose work focuses on maternal, newborn, and child health. Waiswa ranked among Makerere’s overall top researchers after publishing 43 peer-reviewed papers in 2025, tying with three-time award winner Prof. Moses Kamya of the School of Medicine in the College of Health Sciences.
His research examines how health systems function at their most fragile moments, including childbirth, early life, and community-level care, addressing questions of equity, service delivery, and health system performance across Africa.
Also recognised was Dr. David Musoke, an Associate Professor of Disease Control, whose 25 publications earned distinction among senior career researchers. His work spans environmental health, community health systems, and implementation research, areas increasingly viewed as critical to preventing disease before it reaches hospitals.

In the early-career category, Juliana Namutundu received recognition for emerging research leadership, reflecting Makerere’s effort to nurture the next generation of African scholars.
Together, the awards underscored MakSPH’s growing influence within Makerere’s research ecosystem, particularly in fields linking science directly to population wellbeing.

The Research Excellence Awards were established to encourage publication in high-impact journals while reinforcing Makerere’s ambition to become a globally competitive research university. Nominations are reviewed by the Board of Research and Graduate Training, chaired by Deputy Vice-Chancellor (Academic Affairs) Prof. Sarah Ssali.
Awardees were honoured during a graduation luncheon organised by the Makerere University Convocation, the institution’s alumni and staff association, which described the event as a celebration of “excellence and inspiring impact.”
The ceremony also recognised forms of scholarship extending beyond traditional academic publishing.
Dr. Geofrey Musinguzi, a research associate at the School of Public Health, was honoured for his book My Journey with Rectal Cancer, an account of diagnosis, treatment, and recovery that blends personal testimony with public health advocacy.
Diagnosed at age 44 while a visiting scholar at the University of Antwerp in Belgium, Musinguzi sought medical care after experiencing persistent symptoms, including rectal bleeding and back pain. His treatment involved surgeries, chemotherapy, radiotherapy, and a year living with a colostomy bag.
Rather than keeping the experience private, he documented it publicly to challenge cancer stigma and encourage early screening. The book, launched at the School of Public Health in August 2024, highlights how lived experience can shape public health awareness alongside scientific research.
The recognition reflects a broader understanding of research impact, one that includes scholarship capable of influencing behaviour as well as policy.

Makerere’s emphasis on research excellence comes as African universities face increasing pressure to produce locally grounded evidence while competing globally for visibility and funding. For MakSPH, whose work spans disease surveillance, environmental health, and health systems research, publication output increasingly serves as both academic currency and development infrastructure.
“These awards are part of our broader effort to position Makerere as a truly research-led institution,” Nawangwe said, adding that scholarship must remain aligned with national and regional priorities.
Health
Makerere’s 76th Graduation Ceremony: CHS showcases research strength with 26 PhD Graduates
Published
1 week agoon
February 26, 2026By
Zaam Ssali
The second day of the Makerere University 76th Graduation Ceremony, held on Wednesday 25th February, marked another proud moment as the institution continues its tradition of academic excellence and national service. Graduands were presented for conferment of degrees and award of diplomas from the College of Health Sciences (CHS), College of Natural Sciences, College of Veterinary Medicine, Animal Resources and Biosecurity and School of Public Health.
The College of Health Sciences presented a total of 746 graduands for conferment of degrees including 26 PhD, 293 Masters, 425 Bachelors and 2 Diplomas. This is a testament to CHS and Makerere University’s contribution in training skilled health professionals and strengthening Uganda’s health systems through education, innovation and research.
Speaking to the congregation, Professor Barnabas Nawangwe – Vice Chancellor, Makerere University welcomed everyone to Day 2 of Makerere University’s 76th Graduation. He congratulated the 9,295 graduands comprising 4,262 (46%) female graduates and 5,033 (54%) male graduands who will be awarded degrees and diplomas through the graduation week; 213 graduands are PhD recipients. He commended the efforts of staff, parents, and sponsors in supporting the students’ journeys.
He reminded the congregation that outstanding researchers were honored on Day 1 of the graduation for excellence in scholarly work and impactful publications, reaffirming the University’ commitment to research productivity and academic distinction. In addition, the Innovation Commercialization Award was also presented, highlighting Makerere’s focus on turning research into practical solutions that address real-world challenges and drive national development.
The Vice Chancellor highlighted the history of the College established in 1924 cognizant of its impact on Uganda’s Health sector and beyond. He said, ‘As the College enters its second century, it is strengthening specialist training to address increasingly complex health challenges’. CHS has introduced fellowship programmes to equip physicians with advanced expertise which are useful in transforming health systems across Uganda and the region. In 2025 alone, 16 fellows graduated in Pediatric Hematology and Oncology, with additional fellowships underway in Newborn Health, Interventional Radiology, Emergency Care Medicine, and Pulmonary and Critical Care Medicine.
Professor Nawangwe also noted the progression of one of the centres of excellence at CHS, the Makerere University Lung Institute (MLI) established a decade ago to address the growing burden of lung disease in Uganda. He said, ‘today, the MLI serves 6,000 patients annually, shapes national policy and has embarked on construction of a new building, signalling a renewed commitment to advancing respiratory health in Uganda and beyond’.
He also reminded the congregation that CHS continues its centennial celebrations, including the upcoming Alumni Dinner Gala on March 6th 2026 to raise funds for refurbishing the iconic Davis Lecture Theatre, culminating in the unveiling of a Centennial Monument later this year.
Professor Nawangwe applauded the steady advancement of Makerere University into a research-led institution, generating knowledge that drives communities, strengthens industries, and advances national transformation.
Professor Maggie Kigozi was the commencement speaker for Day 2. Professor Kigozi, a distinguished alumna reflected on how her time at Makerere University shaped her life, career, and values, recalling her graduation in 1976 during a period of national uncertainty. Forced to leave Uganda soon after with little more than her education and determination, she noted that her Makerere training opened doors across the region, enabling her to serve in leading health institutions in Zambia, Kenya, and Uganda. Addressing the graduands, she emphasized that their Makerere education remains a powerful passport to opportunity and carries with it the responsibility to uphold excellence and integrity wherever they serve.
She urged graduates in the health and life sciences to handle the power of their profession with humility, compassion, and responsibility, reminding them that behind every patient, case, or experiment lies a life deserving dignity. Beyond clinical expertise, she encouraged them to develop business and financial skills to build sustainable health services and create opportunities for others. She also reassured them that failure is part of growth, noting that resilience, continuous learning, and balance in life are essential to meaningful success as they step forward as ambassadors of the Makerere legacy.
Delivering a speech on behalf of the First Lady and Minister of Education and Sports, Janet Kataha Museveni, the State Minister for Primary Education, Hon. Dr. Joyce Moriku Kaducu, said the Government had deliberately deepened investment in higher education to position universities as drivers of national development.
Hon. Kaducu described the establishment of the Makerere University Research and Innovation Fund (RIF) as a major milestone, noting that it supports high-impact research aligned to national priorities and has enabled thousands of researchers to deliver practical solutions benefiting communities across Uganda. She also highlighted Parliament’s approval of a 162 million US dollar concessional loan from the Korea EXIM Bank to upgrade science, technology and innovation infrastructure at Makerere University, including modern laboratories, smart classrooms and advanced facilities for engineering and health sciences, to better prepare students for the Fourth Industrial Revolution.
The Minister announced plans to construct a national stadium at Makerere and other higher education institutions to promote sports development and talent identification. She reiterated the directive for all universities to fully implement Competence-Based Education and Training by July 2027, urging Makerere to lead curriculum reform, staff training and infrastructure development while ensuring satellite campuses meet full accreditation and uphold academic standards, transparency and accountability.
Addressing graduates, Hon. Kaducu encouraged them to become job creators in sectors such as agriculture, infrastructure, healthcare and education, and to leverage opportunities like the Parish Development Model for entrepreneurship. She commended Makerere’s leadership and partners and congratulated the Class of 2026 on their achievement.
In his address to the congregation, Dr. Crispus Kiyonga – Chancellor, Makerere University congratulated graduands upon making it to the 76th Graduation Ceremony of Makerere University. He described their achievement as a milestone in both personal growth and national development, urging them to apply their knowledge creatively to benefit society. He acknowledged the contribution of academic staff, administrators, the University Council, and expressed gratitude to the Government of Uganda and President Yoweri Kaguta Museveni for continued support.
Dr. Kiyonga called on the university community to strengthen research, expand private sector partnerships, and leverage technology to address Uganda’s development challenges. Emphasising research as central to national progress, Dr. Kiyonga noted the Government’s UGX 30 billion investment annually in the Makerere University Research and Innovation Fund (MakRIF) and praised the Science, Technology and Innovation Secretariat, Office of the President for supporting initiatives at the University advancing homegrown solutions to national challenges. He also highlighted a strengthened partnership with the Korean government, securing a USD 162 million loan from the Korea Exim Bank to boost infrastructure and staff capacity.
While acknowledging limited formal employment opportunities, he encouraged graduates to innovate and create jobs. He further commended the university’s digitalization efforts and outlined four priorities: increased research funding, private sector collaboration, community engagement, and effective use of technology.
During the 76th graduation ceremony running from the 24th -27th February, 2026, a total of 9,295 graduands will be awarded degrees and diplomas in various disciplines. Of these, 213 will receive PhDs, 2,503 Masters Degrees, 206 postgraduate Diplomas, 6343 Bachelor’s Degrees and 30 Diplomas. 46% of the graduands are female and 54% are male.
Trending
-

 General2 days ago
General2 days agoCall for Applications: Diploma Holders under Government Sponsorship 2026/2027
-

 General2 days ago
General2 days agoAdvert: Admissions for Diploma/Degree Holders under Private Sponsorship 2026/27
-

 Humanities & Social Sciences2 weeks ago
Humanities & Social Sciences2 weeks agoMeet Najjuka Whitney, The Girl Who Missed Law and Found Her Voice
-

 General2 weeks ago
General2 weeks ago76th Graduation Highlights
-

 Agriculture & Environment1 week ago
Agriculture & Environment1 week agoCAES Presents Overall Best Performing Student in the Sciences & a Record 28 PhDs at the 76th Graduation Ceremony
